Imagine taking a muscle relaxant for a bad back spasm, then getting prescribed ciprofloxacin for a urinary tract infection. Sounds harmless, right? It’s not. Combining tizanidine and ciprofloxacin can send your blood pressure crashing and knock you out cold-sometimes hard enough to land you in the hospital.
What’s Really Happening in Your Body?
Tizanidine works by calming your central nervous system to reduce muscle stiffness. It’s effective, but it doesn’t last long. Your liver breaks it down quickly-almost entirely using one enzyme: CYP1A2. That’s fine… unless something blocks it. Ciprofloxacin, a common antibiotic for infections like UTIs or sinusitis, is a strong CYP1A2 inhibitor. When you take both, ciprofloxacin shuts down the main path your body uses to clear tizanidine. The result? Tizanidine doesn’t get broken down. It piles up in your bloodstream. Studies show levels of tizanidine can jump 10 to 33 times higher than normal. That’s not a little extra drowsiness. That’s a medical emergency waiting to happen.The Real Risks: Low Blood Pressure and Deep Sedation
When tizanidine surges in your blood, two things happen fast:- Your blood pressure drops dangerously low-sometimes below 70 mm Hg systolic. You might feel dizzy, nauseous, or faint. In severe cases, you pass out, fall, and injure yourself.
- Your brain slows down. You’re not just sleepy-you’re sedated. Some people can’t stay awake, even when spoken to. Others report feeling like they’re in a fog for hours.
Why Tizanidine? Why Not Other Muscle Relaxants?
Not all muscle relaxants behave like tizanidine. Cyclobenzaprine, for example, is broken down by multiple liver enzymes. Even if one pathway gets blocked, others can still clear the drug. That’s why mixing cyclobenzaprine with ciprofloxacin doesn’t cause the same spike in blood levels. Tizanidine is uniquely vulnerable because it relies almost entirely on CYP1A2. There’s no backup. No safety net. That’s why experts call this one of the most dangerous drug interactions in routine practice.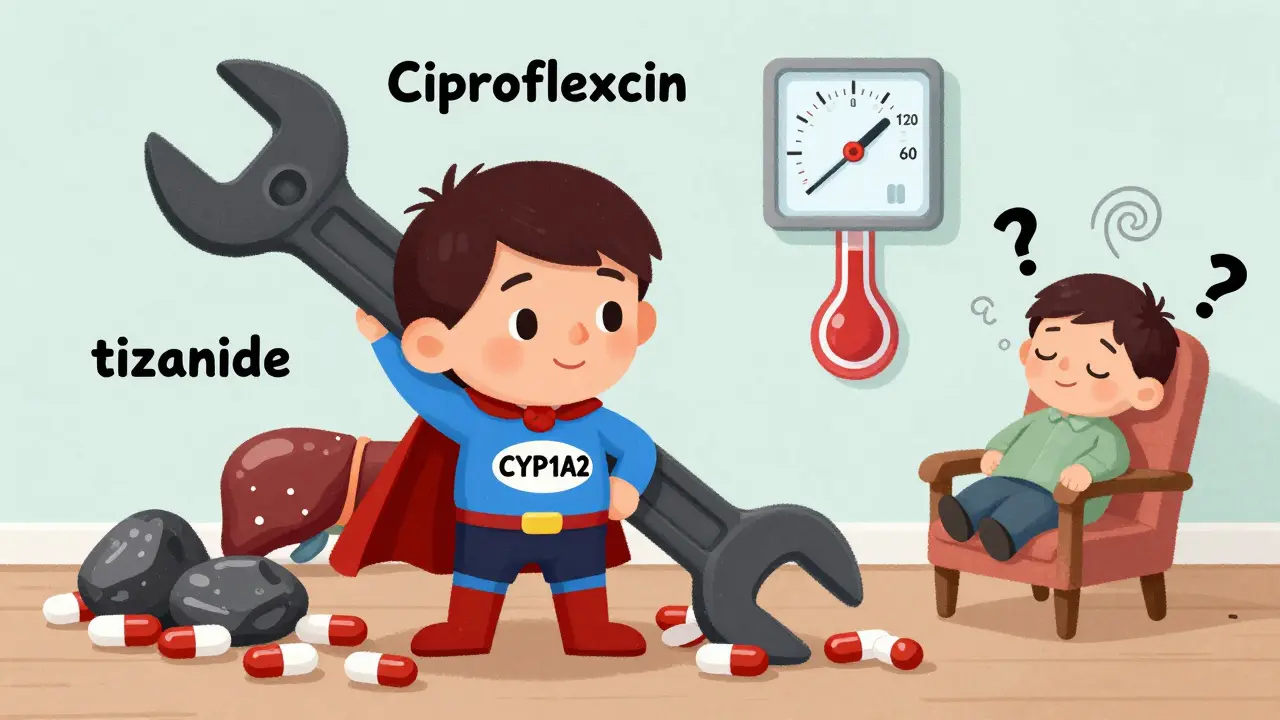
What Do the Experts Say?
The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) both list this combination as contraindicated. That means they officially say: don’t do it. Yet, studies show doctors still prescribe them together. Why? Because the conditions overlap. Someone with chronic back pain gets a UTI. The doctor prescribes ciprofloxacin. The patient’s on tizanidine. No one connects the dots. Clinicians at Vanderbilt University Medical Center found this mix-up happens more often than it should-even after warnings were added to drug labels. They concluded: “Clinicians should avoid co-prescribing these medications.” Dr. Cecilia Chung, who led that research, says the risk isn’t worth it. “The benefits of combining these drugs are negligible. The risks are life-threatening.”What Should You Do?
If you’re on tizanidine and your doctor prescribes ciprofloxacin:- Ask: “Is there another antibiotic I can take?”
- Alternatives like amoxicillin, nitrofurantoin, or doxycycline don’t interfere with CYP1A2 and are just as effective for many infections.
- If ciprofloxacin is absolutely necessary, stop tizanidine during the course of treatment-and for at least 5 to 7 days after.
- Don’t restart tizanidine without talking to your doctor. Your body needs time to clear the antibiotic fully before resuming.

How to Prevent This in the Future
This interaction is preventable-but only if you’re proactive.- Always tell every doctor you see what medications you’re taking-including over-the-counter drugs and supplements.
- Ask your pharmacist to check for interactions every time you get a new prescription.
- Use apps or tools that alert you to dangerous combinations. Many pharmacy apps now flag this specific interaction.
- If you’ve had this combo before and felt unwell, make a note in your medical record. Say: “History of severe reaction to tizanidine + CYP1A2 inhibitors.”
What About Other CYP1A2 Inhibitors?
Ciprofloxacin isn’t the only problem. Other drugs that block CYP1A2 can cause the same reaction:- Fluvoxamine (an antidepressant)
- Ciprofloxacin’s cousin, enoxacin
- Oral contraceptives (in some people)
- Some herbal supplements like St. John’s Wort (in high doses)
The Bigger Picture
This isn’t just about two drugs. It’s about how medicine still misses obvious dangers. Tizanidine is prescribed millions of times a year in the U.S. Ciprofloxacin is one of the most common antibiotics. The interaction has been known for over a decade. Yet, patients still get hurt. It’s a reminder: just because a drug is approved doesn’t mean it’s safe with everything else. Your body’s metabolism is complex. One tiny enzyme blockage can turn a normal dose into a toxic one. The fix? Better systems. Electronic health records should auto-alert doctors when this combo is prescribed. Pharmacists should be required to screen for it. Patients deserve better protection. Until then, you’re your own best defense. Know your meds. Ask questions. Speak up if something feels wrong.Can I take tizanidine and ciprofloxacin if I space them out by a few hours?
No. The interaction isn’t about timing-it’s about enzyme inhibition. Ciprofloxacin blocks CYP1A2 for days, even after you stop taking it. Spacing doses won’t prevent the buildup of tizanidine. The only safe option is to avoid the combination entirely.
How long does the risk last after stopping ciprofloxacin?
Ciprofloxacin stays active in your system for about 24 to 48 hours after your last dose, but its effect on CYP1A2 can linger longer. To be safe, wait 5 to 7 days after finishing ciprofloxacin before restarting tizanidine. Your liver needs time to restore normal enzyme function.
What are the signs I should go to the ER?
Go to the ER if you experience: sudden dizziness or fainting, confusion or inability to stay awake, chest pain, rapid or irregular heartbeat, or a systolic blood pressure reading below 80 mm Hg. These are signs of dangerous hypotension and require immediate medical attention.
Is there a safer muscle relaxant I can use instead of tizanidine?
Yes. Cyclobenzaprine, methocarbamol, and baclofen are alternatives that don’t rely heavily on CYP1A2. Cyclobenzaprine is metabolized by multiple enzymes, making it much safer when combined with antibiotics like ciprofloxacin. Always check with your doctor before switching.
Can I take tizanidine with other antibiotics?
Some are safe, others aren’t. Avoid all fluoroquinolones (like levofloxacin, moxifloxacin) and drugs known to inhibit CYP1A2. Antibiotics like amoxicillin, azithromycin, and doxycycline are generally safe with tizanidine. Always verify with your pharmacist or doctor before combining any new drug.





11 Comments
Sarah Mailloux
Just had my pharmacist flag this combo last week-I was prescribed cipro for a UTI and was on tizanidine for chronic back pain. She looked me dead in the eye and said, 'You’re lucky you came in.' I didn’t even know this was a thing. Thanks for making me feel less like a dumbass for not asking.
Amy Ehinger
I’ve been on tizanidine for five years after a car accident, and last winter I got pneumonia and was put on cipro. I didn’t think twice about it-until I woke up on the bathroom floor at 3 a.m. with my dog licking my face and my husband screaming for 911. Blood pressure was 68/42. They kept me overnight. I didn’t know the drug was that fragile. Now I keep a list of every med I take in my phone and show it to every provider. No more assumptions.
Dan Mack
They’re hiding this on purpose. Big Pharma doesn’t want you to know how many drugs are just time bombs waiting for one little interaction. Ciprofloxacin was designed to kill bacteria-but also to mess with your liver so you need more pills later. They profit from your collapse. You think this is an accident? It’s a business model.
Amy Vickberg
This is exactly why I started using Medisafe. It flagged this combo before I even filled the script. I called my doctor and asked for amoxicillin instead. He was annoyed but grateful I spoke up. We all need to be our own advocates. You’re not being difficult-you’re being smart.
Niki Van den Bossche
The real tragedy isn’t the interaction-it’s the epistemological collapse of modern medicine. We’ve reduced the human body to a biochemical vending machine, where every enzyme is a button to be pressed, every drug a coin to be inserted. But the soul-your soul-doesn’t metabolize in neat, isolated pathways. It’s a symphony of chaos. And when you force two discordant notes into the same measure, the entire composition shatters. You think you’re just taking pills? No. You’re conducting your own slow-motion autopsy.
Gloria Montero Puertas
Oh, please. You’re all acting like this is some groundbreaking revelation. The FDA warned about this in 2012. The British National Formulary listed it as contraindicated in 2010. If you didn’t know this, you didn’t read the damn label. Or worse-you trusted your doctor like they’re infallible. That’s not ignorance, it’s negligence.
Nat Young
Actually, studies show cyclobenzaprine has a higher risk of anticholinergic side effects in the elderly. And baclofen can cause hallucinations. So you’re swapping one risk for another. Maybe the real problem isn’t the combo-it’s that we’re prescribing muscle relaxants at all for chronic pain. They’re not FDA-approved for long-term use. Ever think of physical therapy instead?
Mike Berrange
Just to clarify: ciprofloxacin inhibits CYP1A2, yes. But tizanidine’s half-life is 2.5 hours. Even with 10x concentration, the peak is still under 6 hours. So if you take cipro at 8 a.m. and tizanidine at 10 a.m., you’re not in danger for 24 hours, as some claim. The real risk is if you’re on daily cipro and keep taking tizanidine. That’s when levels stack. And yes, it’s dangerous. But the hysteria? Overblown.
Crystel Ann
I’m so glad someone finally wrote this. My mom had a similar scare last year. She’s 72, on tizanidine for spinal stenosis, got cipro for a UTI, and ended up in the ER. She’s fine now, but she won’t take any new meds without me sitting with her. I wish we had a system where pharmacists called patients directly when a dangerous combo is prescribed. It shouldn’t fall on us to be detectives.
Nicholas Urmaza
Let me be clear: this interaction is not theoretical. It is documented, quantified, and preventable. The data is clear. The guidelines are explicit. If your provider prescribes this combination, ask them to justify it. If they can’t, get a second opinion. Your life is not a gamble. Medication safety is not optional. Take action now.
RUTH DE OLIVEIRA ALVES
As a clinical pharmacist with over two decades of experience, I can confirm that this interaction remains one of the most frequently overlooked yet potentially lethal combinations in outpatient care. While electronic health record alerts have improved, they are still inconsistent across systems. I routinely counsel patients on this risk-even when the prescribing provider has not. Patient education is not a luxury; it is a necessity. Always verify. Always cross-check. Always speak up.