GLP-1 Nausea Duration Estimator
Track Your Nausea Timeline
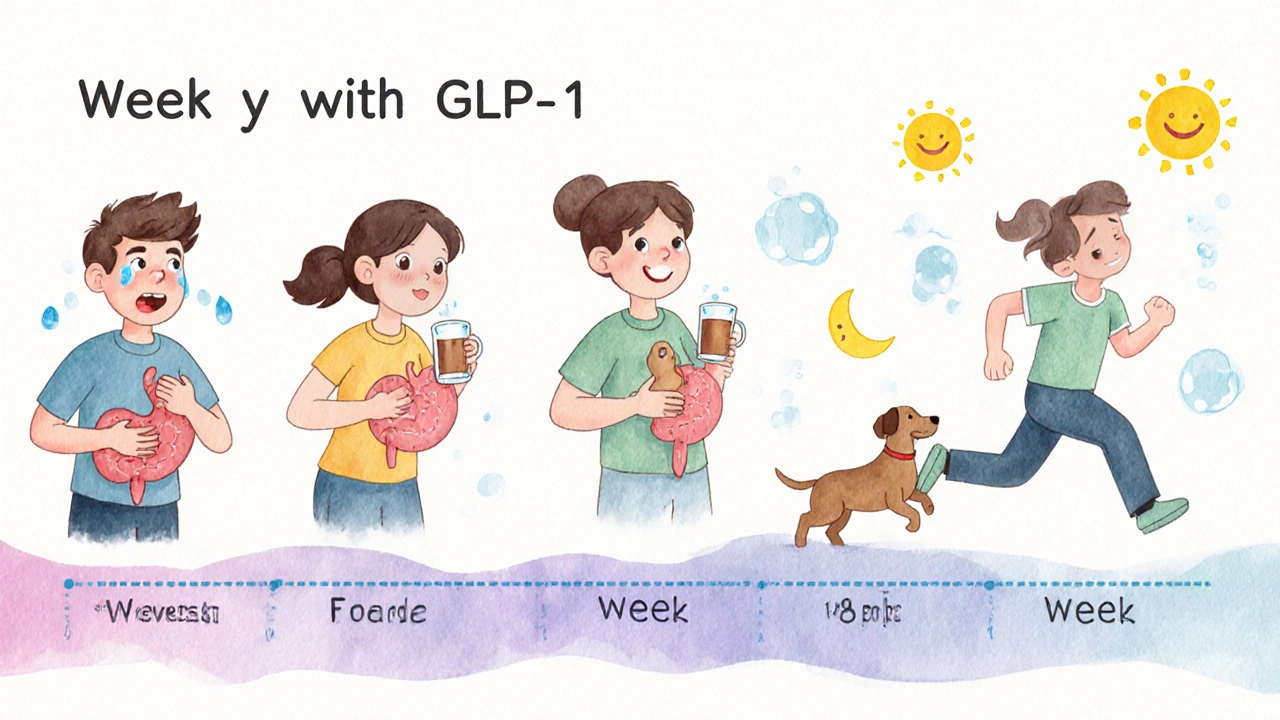
GLP-1 medications like Ozempic, Wegovy, and Mounjaro often cause nausea during the dose-escalation phase. This tool estimates when your symptoms are likely to improve based on your treatment timeline.
Enter your current treatment week to see when nausea typically improves
What This Means
Most patients experience nausea peak around weeks 2-4, with improvement by weeks 6-8. Your body needs time to adjust to the medication. The calculator shows your personalized timeline based on clinical data.
Remember: Symptoms often improve within 2-3 weeks of reaching your maintenance dose. Consistency is key—stopping too early prevents you from experiencing the full benefits.
More than 1 in 8 Americans are now taking a GLP-1 receptor agonist - drugs like Ozempic, Wegovy, or Mounjaro - for diabetes or weight loss. But for many, the benefits come with a heavy price: nausea, vomiting, bloating, and stomach pain. These aren’t rare side effects. They’re the norm. In clinical trials, up to 70% of users reported gastrointestinal issues, and nearly half quit their medication because of them. The good news? Most of these side effects aren’t dangerous, and they usually get better. The key is knowing how to handle them - and when to call your doctor.
Why Do GLP-1 Drugs Make You Feel Sick?
GLP-1 agonists work by mimicking a natural hormone that tells your body to slow down digestion and feel full faster. That’s why they help with weight loss and blood sugar control. But slowing your stomach doesn’t just reduce hunger - it also causes food to sit longer, gas to build up, and your gut to react. The result? Nausea, bloating, constipation, or diarrhea. It’s not a bug - it’s how the drug works. Every GLP-1 medication, whether it’s injected weekly or daily, does this. It doesn’t matter if it’s semaglutide, liraglutide, or tirzepatide. The effect is the same across the board.
When Do Side Effects Start - and Do They Go Away?
Most people feel sick during the first few weeks, especially while the dose is being increased. This is called the dose-escalation phase. For many, nausea hits hardest around week 2 or 3, when the body is still adjusting. But here’s what most people don’t tell you: the worst usually ends by week 6 to 8. A study in the Journal of Clinical Medicine found that over 80% of GI side effects improved or disappeared once patients reached their maintenance dose. That’s why sticking through the first couple of months matters. If you stop too early, you’ll never know if the nausea would’ve faded.
What Are the Most Common Symptoms?
The list is long, but not all of them happen to everyone. Here’s what you’re most likely to experience:
- Nausea - the most common. Feels like your stomach is clenched, with or without vomiting.
- Vomiting - happens in about 20-30% of users, especially early on.
- Diarrhea - loose stools, often linked to faster gut movement in the lower intestine.
- Constipation - slowed digestion can also mean things move too slowly.
- Bloating and gas - your stomach feels full even after small meals.
- Indigestion or stomach pain - dull ache or cramping, usually after eating.
Some people get one symptom. Others get three or four. It varies by person, by drug, and by dose. Higher doses - like those used for weight loss (Wegovy) - tend to cause worse side effects than lower doses used for diabetes (Ozempic).
When to Worry: Red Flags That Need a Doctor
Most GI side effects are annoying, not dangerous. But some signs mean something serious could be happening. If you have any of these, call your doctor right away:
- Severe, constant stomach pain - especially if it’s sharp or radiates to your back.
- Repeated vomiting or diarrhea that lasts more than 2 days.
- Inability to pass gas or have a bowel movement - this could mean a bowel obstruction.
- Yellowing of your skin or eyes (jaundice) - a sign of liver or gallbladder trouble.
- Dark urine, pale stools, or fever along with abdominal pain.
These symptoms are rare, but they’re real. A 2023 JAMA study found GLP-1 drugs increased the risk of pancreatitis, bowel blockage, and gastroparesis (a condition where your stomach can’t empty properly). While these happen in less than 1 in 100 people, they’re serious enough that you can’t ignore them.
How to Reduce Nausea and GI Upset - Proven Tips
You don’t have to suffer through this. Here’s what works, based on real patient experiences and medical advice:
- Go slow with the dose. Your doctor should start you on the lowest dose possible and increase it slowly - often over 16 to 20 weeks. Don’t rush this. Faster escalation means worse nausea.
- Eat smaller meals. Large meals overwhelm your slowed digestion. Try five small meals instead of three big ones.
- Avoid high-fat and fried foods. Fat slows digestion even more, making nausea worse. Stick to lean proteins, vegetables, and whole grains.
- Stay hydrated - but sip slowly. Chugging water can trigger vomiting. Take small sips throughout the day. Try room-temperature water, not ice-cold.
- Don’t lie down after eating. Wait at least 2 hours after a meal before lying down. Gravity helps keep food where it belongs.
- Try ginger. Ginger tea, ginger candies, or capsules have helped many users. It’s a natural anti-nausea remedy.
- Take your dose at night. Many people find nausea is less disruptive if they take the shot before bed. You sleep through the worst of it.
- Use OTC meds if needed. Medications like dimenhydrinate (Dramamine) or meclizine can help with nausea - but only if your doctor says it’s safe.
One Reddit user on r/Wegovy wrote: “I threw up twice in week 3. Then I switched to eating plain oatmeal, sipping ginger tea, and taking my shot at 10 p.m. By week 5, I didn’t even think about it anymore.”
What If the Side Effects Don’t Improve?
If you’ve been on the maintenance dose for 8-12 weeks and nausea, vomiting, or bloating still wreck your days, talk to your doctor. You might need to:
- Stay on your current dose longer - some people need more time.
- Switch to a different GLP-1 drug - semaglutide affects people differently than liraglutide.
- Lower your dose - sometimes, a slightly lower dose still gives good results with fewer side effects.
- Consider a different treatment - there are other diabetes and weight-loss medications without these GI effects.
Don’t feel guilty for quitting. If the side effects are making you miserable, your health isn’t just about the number on the scale or your A1C. Quality of life matters too.
What’s Next for These Drugs?
Researchers are already working on ways to make GLP-1 drugs easier to tolerate. New formulations are being tested that release the drug more slowly, reducing spikes in gut irritation. Some are combining GLP-1 with other agents so lower doses can be used - which could cut side effects in half. The FDA is reviewing several next-gen options expected to hit the market by 2026. Until then, the best tool you have is patience, smart eating, and communication with your care team.
Final Thought: It’s Not All or Nothing
GLP-1 agonists are powerful tools. They help people lose 15-20% of their body weight and lower blood sugar better than almost any other drug. But they’re not magic pills. They’re medications with real, physical effects on your body. The nausea isn’t a sign you’re doing something wrong - it’s a sign the drug is working. The trick is learning to live with it until your body catches up. For many, it gets better. For some, it doesn’t. Either way, you’re not alone. And you’re not weak for needing help.
How long does nausea last on Ozempic or Wegovy?
Nausea usually starts during the dose-escalation phase and peaks around weeks 2-4. For most people, it improves significantly by week 6-8 after reaching the maintenance dose. A small number may have lingering symptoms, but severe nausea lasting longer than 12 weeks is uncommon and should be reviewed by a doctor.
Can I take anti-nausea medicine with GLP-1 agonists?
Yes, but only under medical supervision. Over-the-counter options like dimenhydrinate (Dramamine) or meclizine are often safe and helpful. Avoid herbal remedies or supplements without checking with your provider, as some can interact with your other medications or worsen stomach issues.
Does taking GLP-1 agonists at night help with nausea?
Many users report less nausea when taking their dose at night. This isn’t because the drug works differently - it’s because you sleep through the worst of the symptoms. If you’re struggling with daytime nausea, talk to your doctor about switching your injection time.
Are GI side effects worse with weight-loss doses than diabetes doses?
Yes. Weight-loss doses (like Wegovy) are higher than diabetes doses (like Ozempic), and higher doses mean stronger effects on the gut. Nausea rates jump from about 15-20% at diabetes doses to 30-50% at weight-loss doses. That’s why doctors start everyone on the lowest possible dose and increase slowly.
Should I stop taking GLP-1 agonists before surgery?
Yes. Because these drugs slow stomach emptying, they increase the risk of aspiration during anesthesia. Most surgeons recommend stopping GLP-1 agonists 1-2 weeks before surgery. Always check with your surgical team and prescribing doctor for exact timing.
Do all GLP-1 drugs cause the same side effects?
Yes, the core gastrointestinal side effects - nausea, vomiting, bloating, constipation - are class-wide. Whether it’s semaglutide, liraglutide, or tirzepatide, they all slow digestion. Some people tolerate one better than another, but no GLP-1 drug is free of these effects.
Can GLP-1 agonists cause long-term gut damage?
There’s no evidence they cause permanent gut damage in most people. However, rare complications like gastroparesis or bowel obstruction can occur, especially if symptoms are ignored. Long-term use is still being studied, but current data shows these effects are reversible when the drug is stopped and the gut is given time to recover.





8 Comments
Emily Barfield
Oh my god, I thought I was the only one who felt like my stomach was a rebellious teenager refusing to cooperate… I took Wegovy for 11 weeks, and week 3 was pure horror - I cried while eating toast. But then? I started taking my shot at 11 p.m., ate like a bird, and drank ginger tea like it was holy water… By week 7, I forgot I was even on it. It’s not magic - it’s biology, and patience, and tiny, stupid, beautiful adjustments.
Rahul hossain
One cannot help but observe the alarming normalization of pharmaceutical-induced gastrointestinal distress as a rite of passage for weight loss. One wonders - is this not a society that has come to fetishize suffering as a metric of discipline? The very notion that nausea is 'expected' suggests a profound moral failure in our medical paradigm. We do not applaud the sick for enduring their sickness - yet here we are, applauding the vomiting.
Reginald Maarten
Actually, the claim that '70% report GI side effects' is misleading. That number includes mild, transient nausea - the kind you get from eating bad sushi. The real issue is the conflation of 'common' with 'severe.' In the STEP trials, only 12% of patients discontinued due to 'severe' nausea. Also, 'ginger helps' is anecdotal at best - no RCT has shown statistically significant benefit over placebo for GLP-1-induced nausea. And no, taking it at night doesn't change pharmacokinetics - it just changes your perception of discomfort because you're asleep. Don't mythologize coping mechanisms as cures.
Jonathan Debo
Let’s be clear: if you can’t tolerate the side effects of a GLP-1 agonist, you probably shouldn’t be taking it. This isn’t a yoga class where you ‘listen to your body’ - it’s pharmacology. You want weight loss? Then you accept the trade-offs. The fact that people treat this like a medical emergency is embarrassing. I’ve seen patients cry over bloating while eating a salad. The real problem isn’t the drug - it’s the expectation that medicine should be comfortable. It isn’t. And if you’re too fragile to handle a little nausea, maybe you’re not ready for the responsibility of managing your own health.
Robin Annison
I’ve been on Ozempic for 14 months. The nausea lasted about 7 weeks. What helped most was not ginger or timing - it was changing how I thought about it. Instead of fighting the nausea, I started observing it. Like a cloud passing. I’d say to myself, 'This is the drug working. This is my body adapting.' And somehow, that tiny shift made it bearable. I don’t think it’s about tricks. I think it’s about acceptance. We’re so quick to fix, fix, fix - but sometimes, the medicine is just… being with it.
Abigail Jubb
Okay, but can we talk about how the medical community just… shrugs and says 'it gets better' like it’s a Disney movie? I was on Mounjaro for 10 weeks and I looked like a ghost. My partner had to spoon-feed me broth because I couldn’t keep anything down. I didn’t quit because I was weak - I quit because I was terrified I’d die in the bathroom. And now I’m told I should’ve 'pushed through'? No. That’s not resilience. That’s negligence wrapped in wellness culture.
George Clark-Roden
I read this whole thing twice. And I kept thinking - what if the nausea isn’t the enemy? What if it’s the body’s way of saying, 'Hey, slow down - you’re not just taking a pill, you’re changing your entire relationship with food, with control, with identity'? I’ve seen people lose 30 pounds and still feel empty. The drug doesn’t fix the hunger - it just masks it. Maybe the real question isn’t how to reduce nausea… but why we’re so desperate to silence it. Maybe the nausea is the only honest thing left.
Hope NewYork
lol i took ozempic for 2 weeks and threw up every morning like a drunk college kid. i quit. no regrets. who even needs to be skinny that bad??