FDA Approval: What It Really Means for Your Medications
When you see FDA approval, the U.S. Food and Drug Administration’s official green light for a drug to be sold in the United States. Also known as drug clearance, it means the medication has been tested for safety, effectiveness, and consistent quality before reaching your medicine cabinet. But here’s the thing—FDA approval doesn’t mean all drugs are created equal. Some are brand-new with years of clinical data behind them. Others are generics, made by different companies, often cheaper, and still approved under the same rules. That’s where things get real.
Behind every approved drug is a system called the Orange Book, the official FDA list that rates generic drugs by their therapeutic equivalence to brand-name versions. Also known as Therapeutic Equivalence Evaluations, this is the bible pharmacists use to decide if they can swap your brand-name pill for a generic without risk. Not all generics are equal. Some carry an A code—meaning they’re interchangeable. Others get a B code, which means they might not work the same way, especially for drugs with a narrow therapeutic index like warfarin or levothyroxine. That’s why your pharmacist might flag a substitution, even if the label says "FDA approved." It’s not about trust—it’s about precision.
Then there’s the gap between approval and real-world use. A drug can be approved based on short-term trials but still cause problems months or years later. Think metoclopramide—approved for nausea, but linked to permanent movement disorders. Or ranitidine, pulled from shelves after hidden cancer risks showed up. FDA approval is a starting point, not a finish line. That’s why monitoring side effects, checking for recalls like the Valsartan-Hydrochlorothiazide alert, and understanding therapeutic equivalence codes, the FDA’s system for determining if generics can be safely swapped matters more than ever.
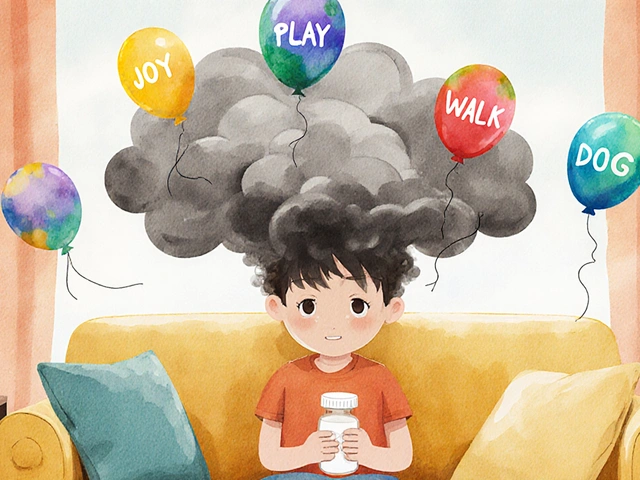
And let’s not forget the role of drug safety, the ongoing process of tracking how medications behave after they’re on the market. Approval doesn’t end when the pill hits the shelf. It’s when patients start using it that hidden risks emerge—like grapefruit messing with statins, or kombucha’s trace alcohol interfering with sensitive meds. The FDA doesn’t just approve drugs. It watches them, updates labels, and sometimes pulls them. You need to watch too.
What you’ll find below isn’t a list of drug ads. It’s a collection of real, practical guides written by people who’ve seen the gaps between approval and outcomes. From how to spot risky generics to why some people need blood tests just to take a common pill, these posts cut through the noise. You’ll learn what FDA approval really means for your health—and how to make sure it works for you, not against you.