When you pick up a prescription at the pharmacy, there’s a 90% chance it’s a generic drug. But how does that pill, tablet, or injection get approved to be sold at a fraction of the brand-name price? The answer lies in the FDA’s Abbreviated New Drug Application (ANDA) process - a system designed to bring safe, effective, and affordable generic medicines to market without repeating every clinical trial ever done.
What Is the ANDA Process?
The ANDA is the legal pathway for generic drug companies to get FDA approval. It’s called “abbreviated” because it doesn’t require the same mountain of clinical data as a brand-new drug. Instead, it builds on the FDA’s previous approval of the original drug - known as the Reference Listed Drug (RLD). If the brand-name drug was approved in 2010 and its patent expired in 2020, a generic maker can submit an ANDA to prove their version works the same way. The whole system was created by the Hatch-Waxman Act of 1984. Before that, generic drugs faced long delays and legal battles. The law gave manufacturers a clear route to market while still protecting innovators’ patents. Today, it’s the backbone of America’s affordable drug supply.How the ANDA Process Works
Getting an ANDA approved isn’t quick or easy, but it’s predictable. Here’s how it breaks down:- Submission: The company files electronically using the FDA’s Electronic Submission Gateway. They include Form FDA-356h (the application) and Form FDA-3674 (financial disclosures).
- Filing Review: Within 60 days, the FDA checks if the application is complete. If it’s missing key data - like bioequivalence results or manufacturing details - it gets sent back.
- Discipline Reviews: Teams of scientists review different parts: chemistry, manufacturing, labeling, microbiology, and bioequivalence. Each team looks for one thing: Is this generic exactly the same as the brand?
- Information Requests: If something’s unclear, the FDA sends an Information Request (IR). This is where most delays happen. Companies often get 10 to 20 IRs before approval.
- Approval or Tentative Approval: If everything checks out and there are no patent or exclusivity blocks, the FDA gives Final Approval. If there’s a patent still in effect, they issue Tentative Approval - meaning the drug is ready to go as soon as the patent expires.
What Makes a Generic Drug “Equivalent”?
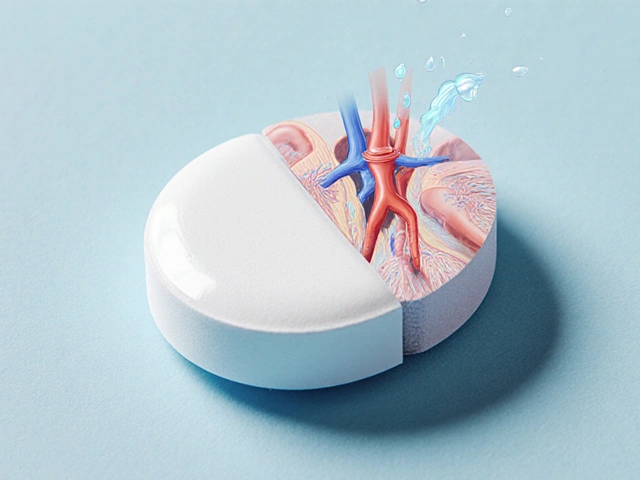
The FDA doesn’t just say, “It looks the same.” They demand proof. For a generic to be approved, it must match the brand in five key ways:- Active ingredient: Same chemical compound, same amount.
- Strength: Same dosage per pill or milliliter.
- Form: Tablet, capsule, liquid, injection - identical.
- Route of administration: Taken by mouth, injected, inhaled - same method.
- Labeling: Same warnings, directions, and uses - with minor exceptions.
Why Is the ANDA Process So Important?
In 2023, generic drugs saved the U.S. healthcare system $373 billion. That’s not a guess. It’s from the FDA and IQVIA. Generics make up 90% of prescriptions but only 23% of drug spending. That’s because a brand-name drug might cost $500 a month - the generic version? $20. This isn’t just about savings. It’s about access. Without the ANDA process, millions of people couldn’t afford their medications. Diabetics, heart patients, people with mental health conditions - they rely on generics to stay on treatment. The FDA’s Office of Generic Drugs (OGD) approved over 1,100 ANDAs in 2022, with a 91% first-cycle approval rate. That’s a high success rate - but only for those who do it right.Challenges Generic Companies Face
Even with a clear process, companies run into roadblocks:- Complex generics: Products like inhalers, patches, or injectables are harder to copy. Bioequivalence studies cost $1 million or more per attempt.
- Patent thickets: Brand companies sometimes file dozens of minor patents to delay generics. This can push approval back for years.
- Facility inspections: The FDA must inspect every manufacturing site. If a plant in India or China fails inspection, the ANDA stalls.
- Information Requests: 78% of applicants report getting unexpected IRs. One company got 17 IRs on their first ANDA - delaying approval by 14 months.
Who’s Winning in the Generic Market?
The U.S. generic market was worth $127.6 billion in 2022 and is expected to hit $189.2 billion by 2027. A few big players dominate:- Teva Pharmaceuticals: Holds 22% of the market. They’ve filed over 1,000 ANDAs.
- Viatris (formerly Mylan): 15% market share.
- Sandoz: 12% market share.

How to Improve Your Chances of Approval
If you’re a generic manufacturer, here’s what works:- Use pre-ANDA meetings: 78% of successful applicants meet with the FDA before submitting. It’s free. It saves time.
- Follow product-specific guidances: The FDA has over 2,000 of these. They tell you exactly how to test your product. Ignore them at your peril.
- Adopt Quality by Design (QbD): 68% of top manufacturers use QbD - building quality into the process, not just testing it at the end.
- Prepare for inspections: Don’t wait until the FDA shows up. Audit your own facility like they’re coming tomorrow.
The Future of the ANDA Process
The FDA is changing. They’re focusing more on complex generics. In 2022, 35% of pending ANDAs were for tricky products like inhalers or topical gels. The agency is investing in new tools - like AI to analyze chemistry data - and real-world evidence to speed up reviews. GDUFA III (effective 2022) pushes the FDA to meet tighter timelines. But the real challenge isn’t the process - it’s the barriers around it. Patent extensions, REMS restrictions, and supply chain issues still block access. Still, the system works. It’s not perfect. But it’s the reason why your insulin, your blood pressure pill, your asthma inhaler costs a fraction of what it did 20 years ago.What’s the difference between ANDA and NDA?
An NDA (New Drug Application) is for brand-name drugs and requires full clinical trials proving safety and effectiveness. An ANDA is for generics and only needs to prove bioequivalence to an already-approved drug. NDA costs around $2.3 billion to develop; ANDA costs $1-5 million.
Can a generic drug be different from the brand?
Legally, no. The active ingredient, strength, dosage form, route, and labeling must be identical. Inactive ingredients (like fillers or dyes) can differ, but they can’t affect how the drug works. The FDA requires bioequivalence testing to prove the body absorbs the drug the same way.
Why do some generics take longer to approve than others?
Complex generics - like inhalers, injectables, or topical creams - are harder to test. They require more sophisticated studies, multiple iterations, and sometimes new analytical methods. The FDA has fewer experts for these products, so reviews take longer. Simple tablets? Often approved in under a year. Complex ones? Can take 5+ years.
What is Tentative Approval?
Tentative Approval means the FDA has found the generic meets all scientific standards - but it can’t be sold yet because of a patent or exclusivity period on the brand-name drug. Once the patent expires, the approval becomes final, and the generic can hit the market immediately.
How long does it take to prepare an ANDA?
Typically 12 to 18 months. This includes developing the manufacturing process, running bioequivalence studies, writing labeling, and compiling the application. Companies often start planning years in advance, especially if they’re targeting a drug with a patent expiring soon.
Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generics to meet the same quality, strength, purity, and stability standards as brand-name drugs. They’re made in the same type of facilities and inspected using the same rules. Millions of patients use generics every day without issue.
Why don’t all drugs have generics?
Some drugs are too complex to copy, like biologics or very small-molecule drugs with tricky delivery systems. Others are protected by patents or exclusivity periods. Also, if the market is too small, companies won’t invest the $1-5 million needed to file an ANDA.
Does the FDA inspect generic drug factories?
Yes. Every manufacturing site - whether in the U.S., India, China, or elsewhere - must pass an FDA inspection before approval. About 63% of ANDA delays are caused by inspection issues. The FDA inspects over 3,500 facilities globally each year.



8 Comments
Matthew Karrs
They say generics are the same, but have you ever seen the side effect reports? I’ve been on the same generic for 3 years and my anxiety spiked every time I switched batches. The FDA doesn’t test how your body reacts to fillers - they just check if the pill dissolves at the same rate. That’s not science, that’s corporate math.
And don’t get me started on the Indian factories. I’ve read the inspection reports. Half of them get flagged for contamination. But hey, $20 pills, right? Someone’s gotta pay the price.
They’re not saving us money - they’re outsourcing risk. And we’re the guinea pigs.
Gerald Cheruiyot
It’s wild how we treat medicine like a commodity. The ANDA process is actually brilliant - it cuts out the redundancy without cutting corners. We’re not just saving money, we’re saving lives. People forget that 90% of prescriptions being generic means millions aren’t choosing between food and insulin.
It’s not perfect. But it’s one of the few systems where regulation actually works for the public. The real villain isn’t the FDA - it’s the patent trolls and the supply chain chaos.
Michael Fessler
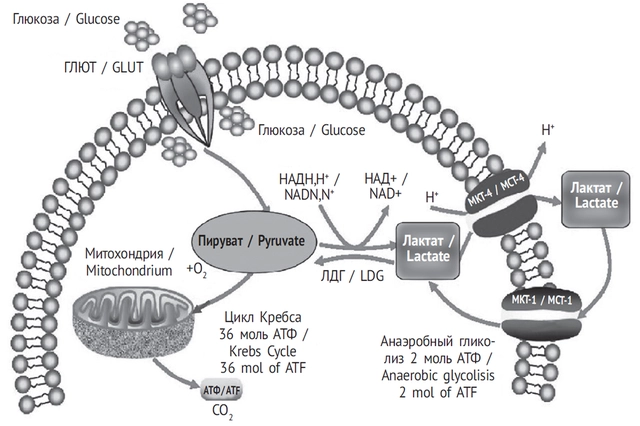
Just to clarify - bioequivalence isn’t just about AUC and Cmax, it’s about the entire PK/PD profile. Most people don’t realize that for complex generics like inhalers, you need in vitro-in vivo correlation (IVIVC) models, which take years to validate. The FDA’s GDUFA timelines are optimistic because they assume perfect submissions.
And yeah, IRs are brutal. I’ve seen companies get stuck on minor labeling discrepancies - like using ‘mg’ vs. ‘milligrams’ - because the reviewer’s team is understaffed. It’s not incompetence, it’s systemic underfunding.
Also, QbD isn’t just a buzzword. It’s the difference between a 30-month review and a 12-month one. If you’re not designing quality into the process, you’re just gambling.
daniel lopez
They’re lying to you. The FDA doesn’t approve generics as safe - they approve them as ‘similar enough’ to avoid lawsuits. The real reason generics are cheaper? Because they’re made in factories with no OSHA oversight, using cheaper solvents, and the active ingredient is often 8-12% off-spec. You think the FDA checks every batch? They check one per year.
And don’t tell me about ‘millions of patients’ - I know a guy who had a seizure after switching to a generic blood thinner. The label didn’t even warn him.
This isn’t healthcare. It’s a corporate Ponzi scheme disguised as regulation. Wake up.
Destiny Annamaria
My grandma takes 7 different generics. She says the only difference she notices is the pill color - and she’s 82. She’s been on them for 15 years. If they were dangerous, don’t you think someone would’ve noticed by now?
Also, the fact that the FDA approved over 1,100 last year means they’re doing something right. I don’t care if it’s a brand or generic - I just want my meds to work without bankrupting me.
Also, Teva’s CEO just donated $10M to free clinics. So maybe they’re not all evil.
Alyssa Torres
Can we just take a second to applaud the scientists behind this? I know it’s boring, but imagine spending 5,000 hours on a single application, running 17 bioequivalence studies, rewriting labeling 12 times, and then getting a 17-point IR because someone used ‘tablet’ instead of ‘tablette’ in the appendix.
This isn’t just bureaucracy - it’s a symphony of precision. And when it works? Someone gets to breathe. Someone gets to take their insulin. Someone gets to live.
So yeah, it’s slow. But it’s sacred work.
Thank you to the people who do this quietly. You’re heroes.
Summer Joy
OK but did you know that 78% of IRs are just to waste time? The FDA’s budget got cut so they’re forcing companies to redo stuff just to keep their jobs. I read a whistleblower report - they literally train reviewers to nitpick so they look busy.
And the ‘tentative approval’ thing? That’s a trap. Companies spend millions, then sit on it for 3 years while the brand company sues them into oblivion.
Also, I saw a TikTok of a generic pill that looked like a Skittles. That’s not a coincidence. They’re trying to make us feel like we’re taking candy. 🤢
Aruna Urban Planner
Interesting. In India, we have a similar system called the ‘ANDA-equivalent’ under CDSCO, but the timelines are even longer - 4 to 6 years for complex products. The challenge isn’t just science - it’s infrastructure. Labs lack equipment, data integrity is weak, and inspectors are underpaid.
Still, the principle holds: if you can prove equivalence, you shouldn’t need to repeat Phase III trials. It’s rational. The problem is global inequality in enforcement.
Maybe the FDA’s AI tools could be shared with low-income regulators. That’d help more than patents ever did.