Opioids and Depression: How Pain Medications Affect Mood and What to Do
When you take opioids, a class of drugs used to treat moderate to severe pain, including prescription pills like oxycodone and hydrocodone, as well as illicit substances like heroin. Also known as narcotics, they work by binding to receptors in your brain and spinal cord to block pain signals. But for many people, the relief doesn’t stop at pain. Over time, opioids can change how your brain handles mood, motivation, and pleasure—leading to depression, a mental health condition marked by persistent sadness, loss of interest, fatigue, and trouble concentrating. It’s not just in your head—it’s in your chemistry.
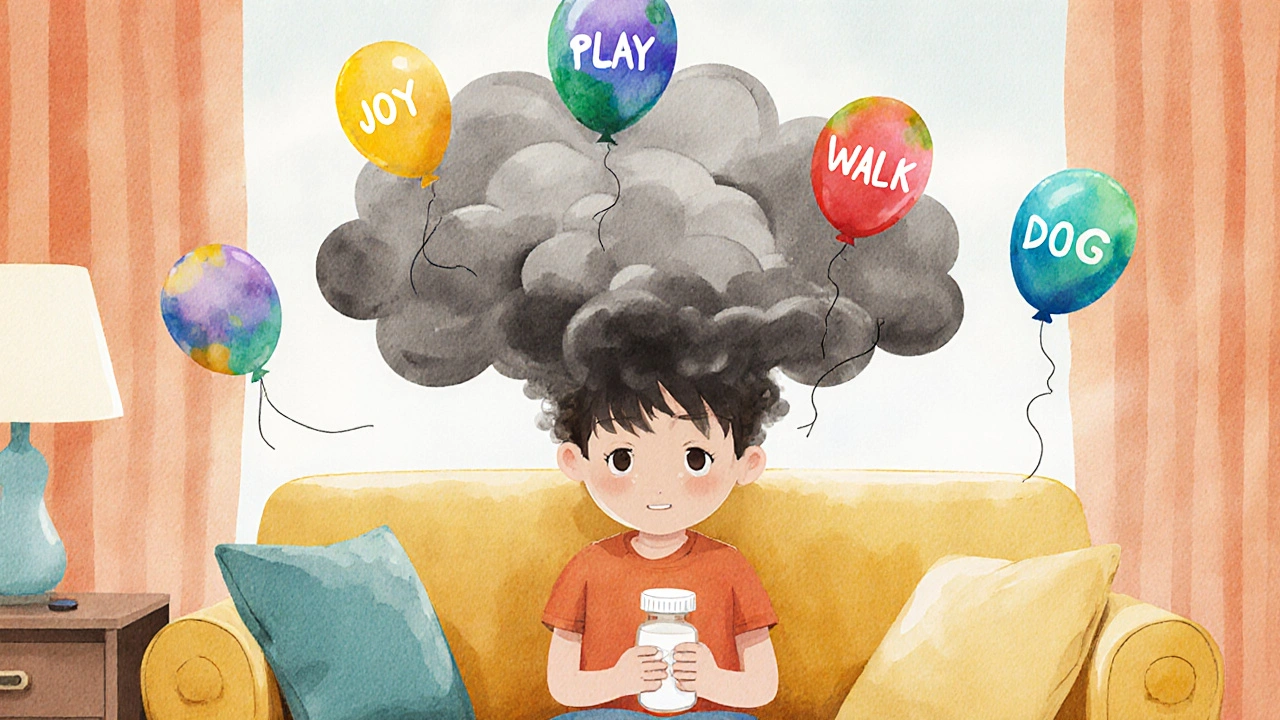
Here’s the catch: people often start opioids for physical pain, but end up struggling with emotional pain too. Studies show up to half of long-term opioid users develop symptoms of depression, even if they never had it before. Why? Opioids flood your brain with dopamine at first, making you feel good. But over weeks or months, your brain stops making its own dopamine. When the drug wears off, you feel flat, numb, or worse. That’s not just withdrawal—it’s a chemical shift that mimics clinical depression. And when you try to quit, the crash can be brutal: low mood, insomnia, anxiety, and a crushing sense of hopelessness. This isn’t weakness. It’s neurobiology.
Some people think switching to an antidepressant will fix it. But that’s not always enough. antidepressants, medications like SSRIs and SNRIs used to treat depression and anxiety, can help with mood, but they don’t reverse the brain changes caused by opioids. And if you’re still taking opioids while on antidepressants, interactions can make things worse—slowing metabolism, increasing sedation, or raising the risk of serotonin syndrome. You need a plan that addresses both the pain and the mood, not just one or the other. That means talking to your doctor about tapering opioids safely, exploring non-opioid pain options like physical therapy or nerve blocks, and pairing it with counseling or support groups that understand the dual struggle.
Depression from opioids isn’t rare. It’s common. And it’s treatable—but only if you recognize it early. If you’ve been on pain meds for more than a few months and notice you’re not enjoying things like you used to, or you’re feeling down even when your pain is under control, don’t brush it off. It’s not just "being sad." It’s your brain adapting to a drug that’s no longer serving you. The good news? Many people recover fully once they stop opioids and get the right support. You don’t have to choose between pain relief and mental health. There are better paths.
Below, you’ll find real guides from people who’ve been there—how to manage side effects, when to question your meds, how to spot early signs of trouble, and what alternatives actually work. These aren’t theoretical tips. They’re the kind of advice you wish you’d heard before you started.