Opioid Use and Mental Health: Risks, Links, and What You Need to Know
When people talk about opioid use, the consumption of prescription or illegal drugs like oxycodone, heroin, or fentanyl that act on the brain’s pain and reward systems. Also known as opioid dependence, it often starts with a legitimate prescription but can quickly spiral into something far more dangerous. What many don’t realize is that opioid use doesn’t just affect your body—it rewires your brain in ways that make mental health conditions like depression, anxiety, and PTSD worse, or even trigger them for the first time.
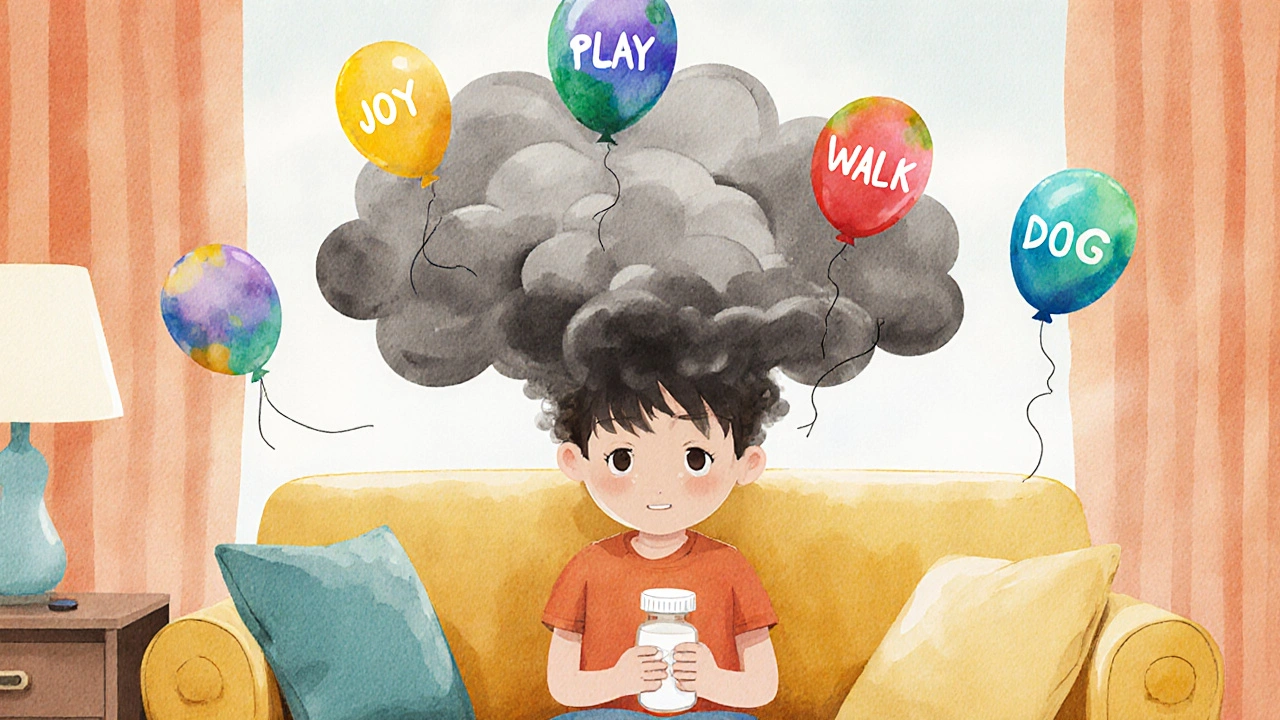
The link between opioid addiction, a chronic condition where a person compulsively seeks and uses opioids despite harmful consequences and mental health, the state of a person’s emotional, psychological, and social well-being isn’t just correlation—it’s cause and effect. People with untreated depression are more likely to misuse opioids to numb emotional pain. At the same time, long-term opioid use lowers dopamine levels, making it harder to feel pleasure from anything else. This creates a loop: you use opioids to feel better, but over time, you need more just to feel normal. And when you try to stop? Withdrawal can feel like a panic attack mixed with deep sadness—and that’s when relapse is most likely.
This isn’t theoretical. Studies show over half of people in treatment for opioid addiction also have a diagnosable mental health disorder. It’s not that one causes the other in a simple way—it’s that they feed each other. Anxiety makes you want to escape. Opioids give temporary relief. But the relief fades, and the anxiety comes back louder. The same goes for trauma. People with PTSD often self-medicate with opioids because the drugs temporarily quiet the noise in their heads. But the brain adapts. The trauma doesn’t go away. The dependency does.
What’s missing from most conversations is that treating just the addiction—or just the mental health issue—rarely works. You need both at the same time. Medications like buprenorphine can reduce cravings and withdrawal, but without therapy to address the root emotional pain, the risk of returning to opioids is high. Support groups, counseling, and sometimes antidepressants are just as important as detox. And yes, it’s possible to recover. But it’s not about willpower. It’s about fixing the broken system inside your brain and learning new ways to cope.
Below, you’ll find real, practical guides from people who’ve been there. From managing side effects of pain meds that worsen anxiety, to understanding how naloxone saves lives but doesn’t fix the deeper struggle, to knowing when to switch from one drug to another without triggering a mental health crisis. These aren’t theoretical articles. They’re tools for people trying to break free—and stay free.