Inflammation: Causes, Symptoms, and Practical Ways to Feel Better
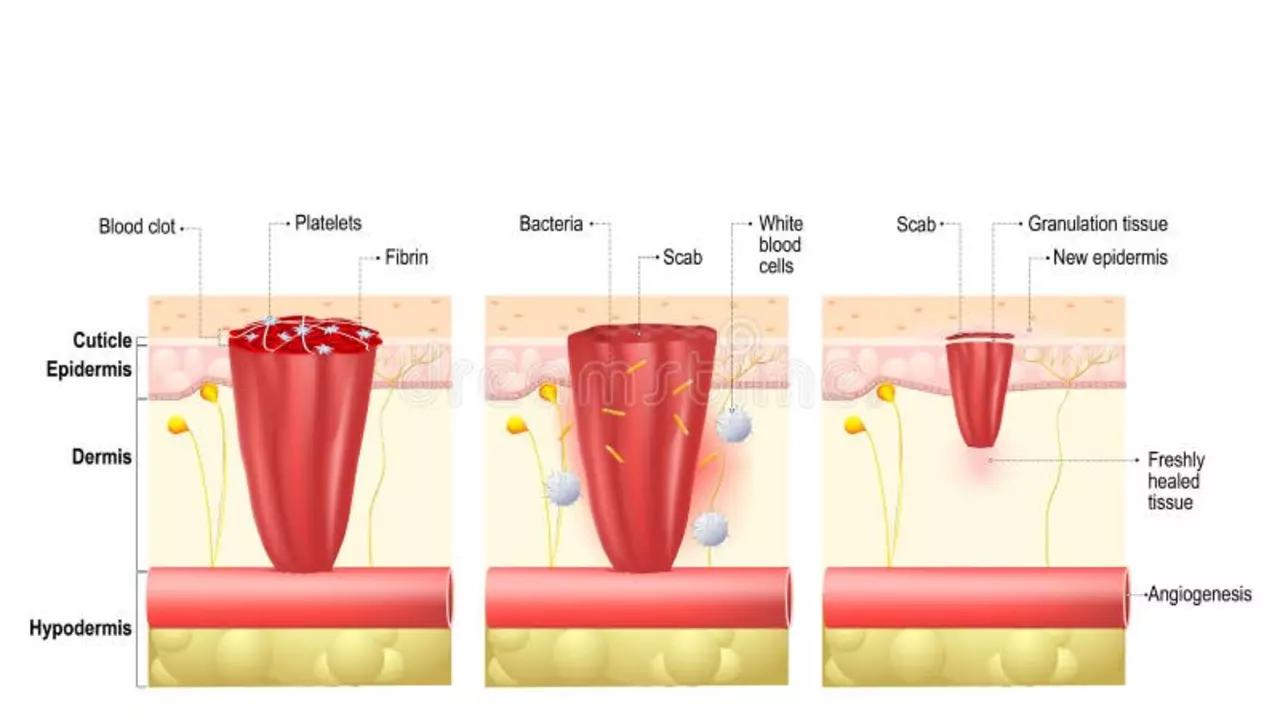
Inflammation isn’t just swelling after a sprain — it shows up in your gut, joints, skin, and even your mood. Acute inflammation is the body's quick response to injury or infection. Chronic inflammation sticks around and quietly damages tissue over months or years. Know which one you’re facing: short-lived pain that follows an injury is different from long-term fatigue, digestive trouble, or joint stiffness that won’t go away.
Common signs to watch for include redness, heat, pain, swelling and loss of function. For internal inflammation you might get tired, have unexplained fevers, persistent digestive symptoms, or worsening allergies. If symptoms interfere with daily life or last more than a few weeks, see a doctor — some causes need tests and targeted meds.
Simple habits that cut inflammation fast
- Move a little every day. Walking, light strength work, or gentle yoga lowers markers like CRP. Start with two 20-minute walks a week and build up.
- Sleep matters. Aim for 7–8 hours and keep a bedtime routine. Poor sleep raises inflammatory hormones.
- Cut sugary drinks and refined carbs. Swap soda for water and whole fruit.
- Add foods that help: fatty fish, walnuts, berries, leafy greens, and turmeric. Real food beats most supplements for steady results.
When medication helps
OTC pain relievers like ibuprofen and naproxen reduce inflammation short-term. For specific conditions, doctors may prescribe drugs tailored to the problem: mesalamine for inflammatory bowel disease, antibiotics like ampicillin for certain infections, or blood pressure meds that double as heart-protective agents. Your treatment depends on the cause, so don’t self-prescribe long-term.
Supplements promise big anti-inflammatory gains, but evidence varies. Turmeric can help a bit, while many herbal blends lack reliable data. If you try a supplement, tell your doctor — some interact with meds or cause side effects.
Practical checklist before you visit a doctor: note when symptoms started and what makes them better or worse. List all meds, supplements, and recent infections. Track sleep, diet, and activity for a week — patterns matter. Bring this info to your appointment to speed up a correct diagnosis.
Common tests your doctor might order include blood CRP or ESR to measure inflammation, full blood count to check infection, imaging like ultrasound or MRI for joint problems, and stool tests if bowel inflammation is suspected. Knowing likely diagnosis speeds treatment. If you have autoimmune signs, your doctor may refer you to a specialist like a rheumatologist or gastroenterologist. Take notes during visits and ask for clear next steps. Start today.
If gut inflammation is your main issue, read our colitis diet guide and the mesalamine article. Curious about infection-driven inflammation? See the ampicillin and sinus infection piece. For heart-related inflammation and blood pressure links, check the Diovan overview. Those pages give condition-specific details and next steps.
If you want one simple rule: reduce daily triggers and get checked when problems persist. Small changes stack quickly and can cut inflammation without heavy drugs.