Understanding the Basics: Blood Clots and Stents
Before we delve into the complex world of blood clots and stents, it's essential to understand the basics. A stent is a small, metal mesh tube that opens up a narrow or blocked artery. They are often placed in arteries during a procedure called angioplasty. On the other hand, a blood clot is a clump of blood that has changed from a liquid to a gel-like or semisolid state. This can be harmful when it forms inside our veins or arteries.
What Causes Blood Clots in Stents?
Various factors can trigger the formation of blood clots in stents. These include the body's natural response to a foreign object, the type of stent used, the patient's health condition, and issues related to stent placement. These factors can lead to a condition known as stent thrombosis, a serious complication where a clot forms in the stent.
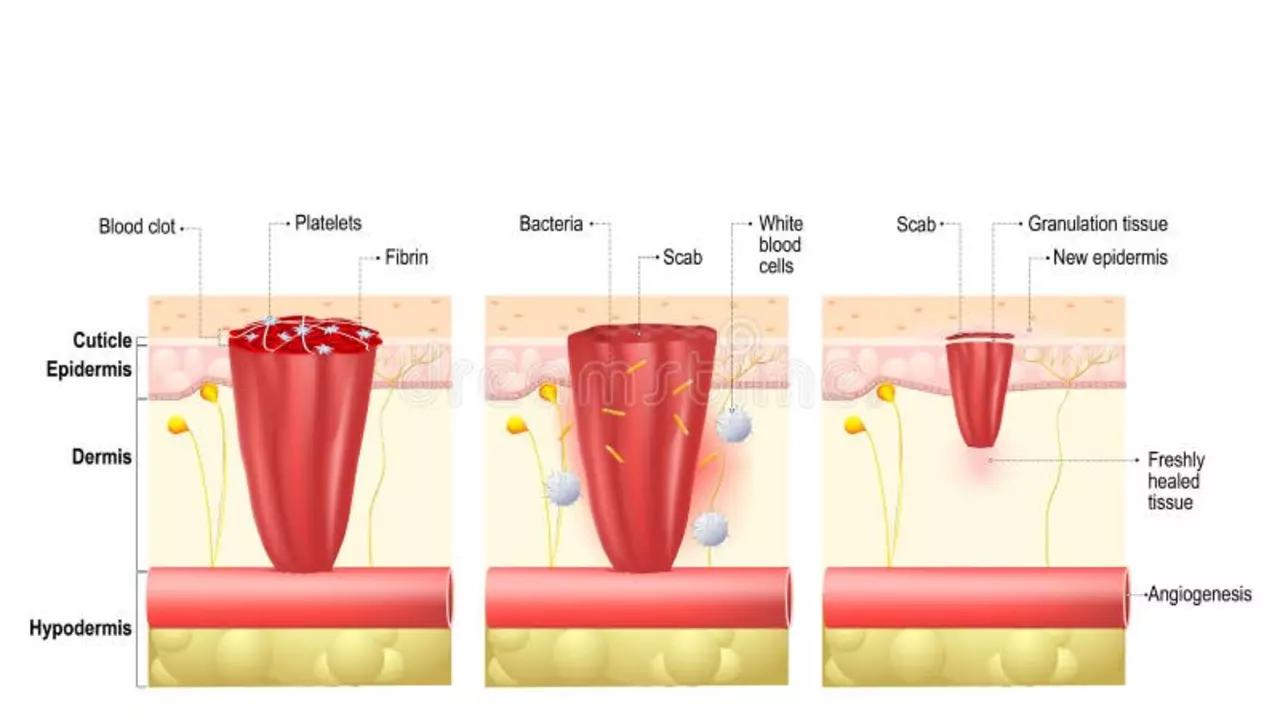
Linking Blood Clots and Inflammation
Under normal circumstances, our body's inflammatory response helps us heal. However, when a stent is placed, this response can sometimes go awry, leading to the formation of a blood clot. Inflammation can cause our blood to become 'stickier' and more likely to clot, promoting the formation of blood clots in stents.
Role of Inflammation in Stent Thrombosis
The role of inflammation in stent thrombosis is complex and multifaceted. When a stent is inserted, it can cause injury to the arterial wall. This triggers an inflammatory response that can lead to the formation of a clot. Furthermore, the stent itself can act as a foreign body, triggering an inflammatory response that can also promote clotting.
Negative Effects of Blood Clots in Stents
Blood clots in stents can have serious consequences. The most significant risk is that the clot can block blood flow through the artery, leading to a heart attack or stroke. Even small clots can be dangerous, as they can break off and travel to other parts of the body, causing damage to other organs.
Preventing Blood Clots in Stents
Given the potential dangers of blood clots in stents, it's crucial to take steps to prevent them. These include taking antiplatelet medications as prescribed, maintaining a healthy lifestyle, and having regular check-ups with your doctor. It's also important to be aware of the signs and symptoms of a clot, so you can seek immediate medical attention if needed.
Role of Anti-Inflammatory Medications
Anti-inflammatory medications can play a key role in preventing blood clots in stents. By reducing inflammation, these drugs can help to reduce the 'stickiness' of the blood and decrease the likelihood of a clot forming. However, these medications must be taken under the supervision of a doctor, as they can have side effects.
Understanding the Inflammation-Clot Connection
Understanding the connection between inflammation and blood clots can help us to better manage and prevent complications related to stents. By controlling inflammation, we can help to reduce the risk of blood clots, and by extension, the risk of heart attacks and strokes.
Further Research into Inflammation and Blood Clots in Stents
Despite the progress that has been made in understanding the role of inflammation in blood clots in stents, there is still much to learn. Ongoing research is crucial to further our understanding of this complex issue and to develop new and better ways to prevent and treat blood clots in stents. With continued research and innovation, we can hope for a future where the risks associated with stents are minimized.




7 Comments
Annette Smith
Stents are tiny metal scaffolds that keep arteries open. When we put a foreign object inside a blood vessel, the body can see it as a threat. That threat often triggers inflammation, which makes the blood more prone to clotting. Over time, this can lead to stent thrombosis, a serious complication. Managing inflammation with medication and lifestyle changes helps keep the clot risk low.
beth shell
I think it’s fascinating how a small mesh can change blood flow dynamics and how our immune system reacts to it. Awareness of the process encourages better compliance with therapy
khushali kothari
The pathophysiology of stent thrombosis involves endothelial disruption, platelet activation, and a cascade of pro‑inflammatory cytokines such as IL‑6 and TNF‑α. Drug‑eluting stents mitigate neointimal hyperplasia but may alter local immune signaling, thereby influencing thrombotic propensity. Moreover, the shear stress alterations at the stent struts potentiate platelet aggregation via von Willebrand factor exposure. Consequently, dual antiplatelet therapy remains the cornerstone of prophylaxis, albeit with individualized duration based on risk stratification.
Brandon Smith
It’s irresponsible to ignore the medical advice surrounding antiplatelet regimens. Skipping doses not only endangers the individual but also burdens the healthcare system with preventable emergencies. Discipline in medication adherence is a moral imperative.
darwin ambil
Stent care is a daily habit, don’t forget your meds 😊
Brian Koehler
Indeed, the integration of anti‑inflammatory pharmacotherapy, alongside antiplatelet agents, constitutes a synergistic strategy; this approach, when coupled with rigorous lifestyle modification-dietary optimization, regular aerobic exercise, and smoking cessation-substantially reduces thrombotic risk; moreover, periodic imaging surveillance, such as intravascular ultrasound, offers valuable insight into endothelial healing and stent patency.
Clinicians should tailor therapy to each patient’s risk profile.
Dominique Lemieux
While the call for strict adherence to prescribed regimens is undeniably valid, the discourse often collapses into a binary of obedience versus negligence, neglecting the nuanced psychosocial landscape that shapes patient behavior. One must consider, for instance, the economic constraints that render prolonged antiplatelet therapy a financial strain for many households, especially in under‑insured populations. Additionally, cultural beliefs about medication can foster skepticism toward pharmaceutical interventions, thereby influencing compliance in ways that are not simply a matter of willpower. The literature, replete with systematic reviews, underscores that shared decision‑making, rather than paternalistic instruction, correlates with higher adherence rates. Moreover, the physiological heterogeneity among patients-variations in platelet reactivity, genetic polymorphisms affecting drug metabolism, and comorbidities such as diabetes-necessitates a personalized pharmacologic blueprint rather than a one‑size‑fits‑all mandate. When clinicians adopt a dialogic stance, inviting patients to articulate concerns, they engender trust and, consequently, a greater likelihood of sustained medication use. It is also worth noting that the risk of bleeding complications, which can be catastrophic, may prompt patients to self‑adjust dosages in an attempt to balance perceived dangers. Such self‑modification, often vilified by moralizing rhetoric, is a rational response to incomplete information. Therefore, the narrative should evolve from shaming language to empathetic education, incorporating clear explanations of risk‑benefit calculus. In parallel, health systems should invest in supportive infrastructures-reminder apps, community health workers, and subsidized medication programs-that alleviate the burden on individual agency. Finally, ongoing research into novel antithrombotic agents with favorable safety profiles promises to simplify the therapeutic algorithm, potentially rendering the current adherence conundrum obsolete. In sum, the path forward lies not in castigating non‑compliance, but in constructing an ecosystem where adherence is the path of least resistance for the patient. Such an ecosystem would integrate multidisciplinary teams, including pharmacists, dietitians, and mental health counselors, all working toward a shared adherence goal. Patient empowerment through education about the mechanistic underpinnings of stent thrombosis can demystify the perceived threat and foster proactive health behaviors. Digital health platforms that provide real‑time feedback on platelet function or inflammatory markers hold promise for personalized adherence monitoring. Ultimately, bridging the gap between clinical guidelines and lived experience requires humility, flexibility, and sustained investment from all stakeholders.