Epilepsy: Practical Guide to Seizure Care and Treatment
About 1 in 26 people will develop epilepsy in their lifetime. If you or someone close to you has seizures, straight answers matter more than medical jargon. This page gives clear, useful steps you can use right away: how to spot seizures, basic first aid, common treatments, and everyday tips to reduce risk.
What epilepsy looks like and when to get help
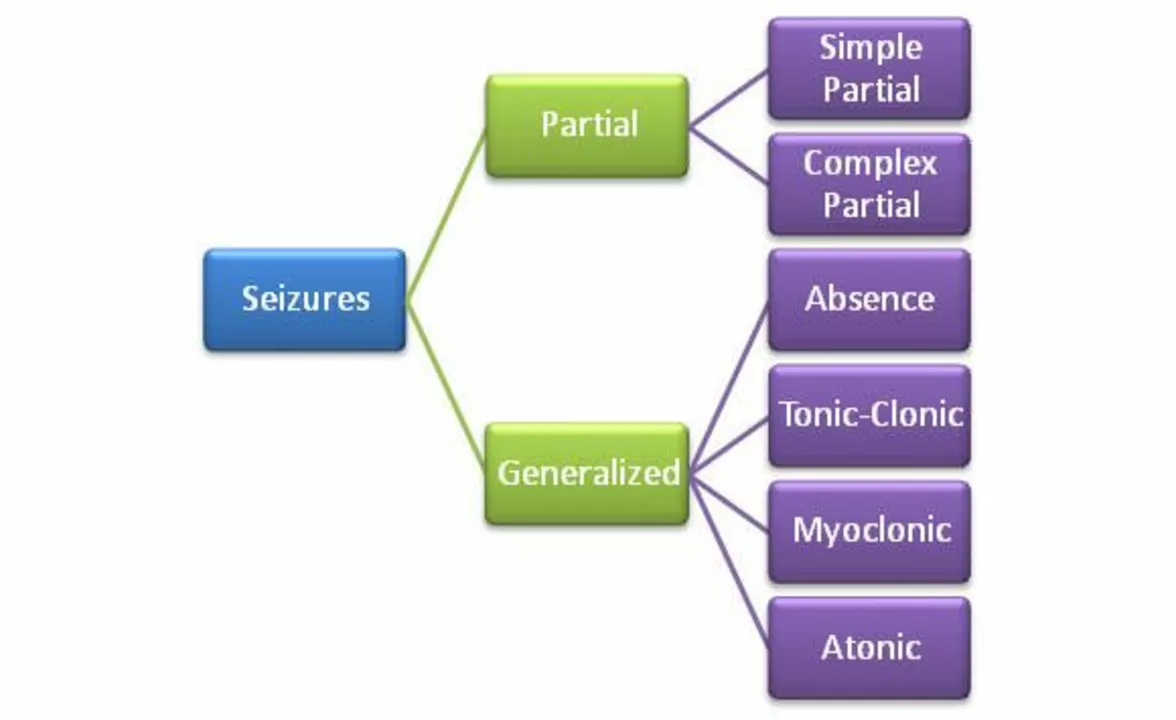
Epilepsy is a tendency to have repeated, unprovoked seizures. Seizures vary: some cause full-body convulsions and loss of awareness, others are brief staring spells or odd sensations. Typical signs include sudden collapse, stiffening or twitching of limbs, drooling, rapid eye movement, or confused behavior after the event.
Call emergency services if a seizure lasts longer than 5 minutes, if the person has repeated seizures without regaining consciousness, if it follows a head injury, if breathing is difficult, or if the person is pregnant or diabetic. For a first-time seizure, seek urgent medical evaluation—tests and medicines may be needed.
Treatments, medicines, and what to watch for
Most people with epilepsy manage it with antiepileptic drugs (AEDs). Common options you’ll hear about include levetiracetam (Keppra), carbamazepine, lamotrigine, and valproate. Each drug works differently and carries its own side effects: fatigue, dizziness, weight or mood changes, and sometimes more serious risks. Valproate requires special caution in women of childbearing age because it raises the risk of birth defects.
Medication adherence is the single most important step you can take. Missing doses is a leading cause of breakthrough seizures. Talk openly with your doctor about side effects, interactions with other drugs or supplements, and whether blood tests are needed to check levels.
If medicines don’t control seizures, other options exist: epilepsy surgery, vagus nerve stimulation (VNS), or newer devices that monitor and respond to brain activity. A specialist (epileptologist) can explain what fits your situation.
Keep a seizure diary—note triggers, sleep, meds, alcohol, and how long each event lasts. This helps your doctor fine-tune treatment.
Daily life: safety, triggers, and support
Practical changes reduce risk. Get enough sleep, avoid heavy alcohol, take meds at the same time daily, and manage stress. For photosensitive epilepsy, use screens with reduced brightness and enable blue-light filters.
Wear ID that says you have epilepsy or carry emergency info. At home, pad sharp corners, avoid unsupervised swimming, and tell close contacts how to help. First aid basics: protect the head, turn the person onto their side once jerking stops, do not force anything into the mouth, and time the seizure. Stay calm and stay with them until fully recovered.
If you're searching for reliable info, bring questions to your doctor and use resources that list evidence-based treatments. Blueskydrugs.com has plain-language guides on medications and safety if you want deeper reading. Above all, don’t manage epilepsy alone—find a care team and a support network to help you stay safe and active.