Bulimia Long-Term Risk Estimator
This tool estimates potential long-term health risks associated with bulimia nervosa based on behavior patterns. Enter your information below:
bulimia nervosa is more than a brief episode of binge‑purge cycles; the damage can linger for years, reshaping both physical health and emotional well‑being. Below you’ll find the most critical take‑aways before we dive into the details.
- Chronic electrolyte loss can trigger heart rhythm problems and kidney strain.
- Repeated stomach stretching leads to permanent gastrointestinal dysfunction.
- Acidic vomit erodes tooth enamel and softens gums, causing long‑term dental disease.
- Hormonal imbalances increase risk of bone loss, infertility, and metabolic slowdown.
- Persistent shame and anxiety often evolve into depression or anxiety disorders.
What is Bulimia Nervosa?
When building a clear picture, start with a definition. Bulimia Nervosa is a serious eating disorder marked by recurring binge‑eating episodes followed by compensatory behaviors such as self‑induced vomiting, laxative misuse, fasting, or excessive exercise. It affects roughly 1‑2% of the population, with higher prevalence among females aged 15‑29, though men are increasingly recognized.
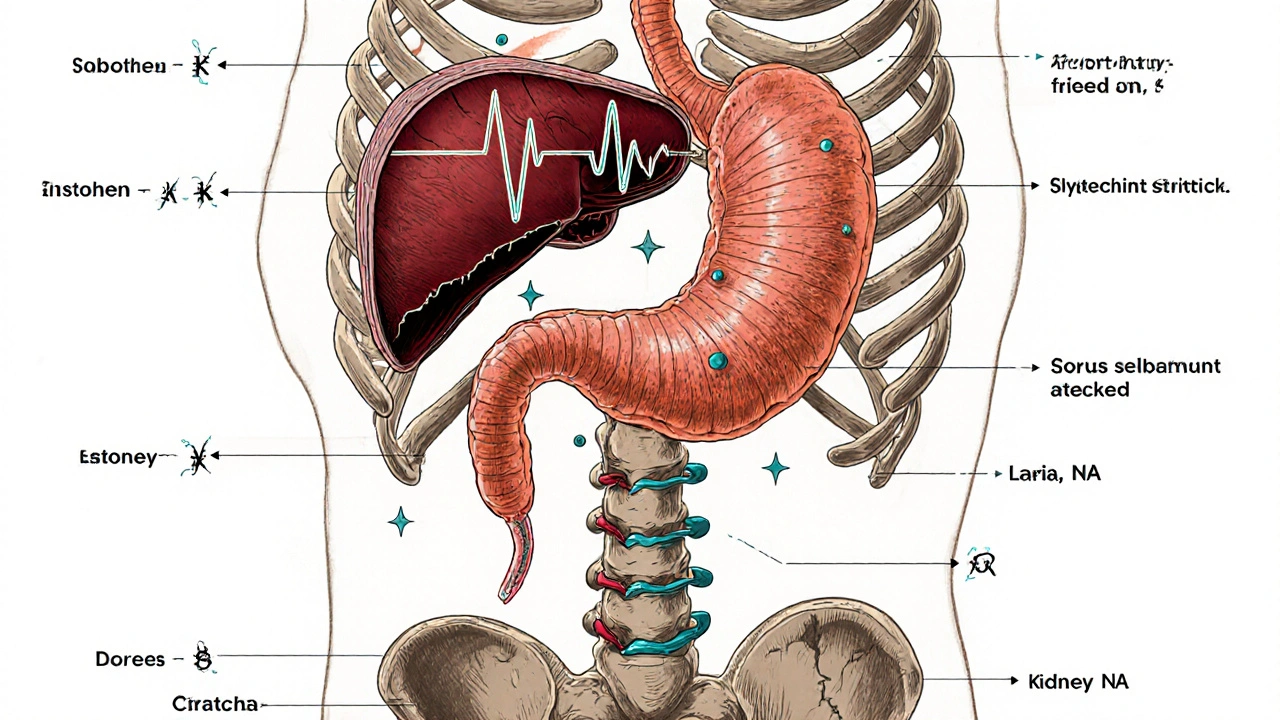
Physical Toll Over Time
The body’s response to frequent purging is a cascade of stressors. Below are the most common organ‑system impacts.
- Electrolyte Imbalance refers to abnormal levels of sodium, potassium, chloride, and bicarbonate caused by vomiting or laxative abuse. Chronic low potassium (hypokalemia) weakens cardiac muscle, leading to Cardiac Arrhythmia irregular heartbeats that can cause fainting, palpitations, or sudden cardiac arrest.
- Gastrointestinal Damage includes repeated stretching of the stomach, esophageal tears, and delayed gastric emptying. Over years, this can evolve into chronic reflux, gastroparesis, and malabsorption.
- Dental Erosion is the loss of enamel due to frequent exposure to stomach acid. Enamel thins, gums recede, and cavities become rampant, often requiring extensive restorative work.
- Osteopenia is reduced bone mineral density that stems from hormonal disruption, nutrient deficiencies, and cortisol excess. Women may face early menopause, while men risk fractures in their 30s.
- Hormonal Dysregulation includes altered leptin, ghrelin, and reproductive hormones, affecting metabolism and fertility.
Mind‑Body Connection
Physical complications rarely exist in isolation. The chronic stress of secretive binge‑purge cycles fuels mental‑health decline.
- Depression affects up to 70% of individuals with bulimia, driven by guilt, low self‑esteem, and neurochemical shifts.
- Anxiety Disorders including generalized anxiety and social phobia, often intensify as purging becomes a compulsive coping tool.
- Cognitive Impairment such as difficulties concentrating, memory lapses, and decision‑making deficits, linked to electrolyte fluctuations and chronic stress hormones.
Typical Long‑Term Complications
| Effect | Short‑Term | Long‑Term |
|---|---|---|
| Electrolytes | Transient hypokalemia, dizziness | Chronic arrhythmia, kidney damage |
| Gastro‑intestinal | Acid reflux, nausea | Gastroparesis, esophageal stricture |
| Dental | Enamel softening | Severe erosion, tooth loss |
| Bone health | Minor calcium loss | Osteopenia/osteoporosis, fractures |
| Mental health | Shame, guilt | Major depressive disorder, chronic anxiety |
Managing and Reducing Risks
Early intervention is key, but even after years of struggle, recovery can halt further damage.
- Seek a multidisciplinary team: a therapist specialized in eating disorders, a dietitian, and a medical doctor familiar with electrolyte monitoring.
- Regular labs: full metabolic panel every 3‑6months to catch potassium, chloride, magnesium, and renal function trends.
- Dental care: fluoride treatments and night‑guard usage to protect enamel while the body heals.
- Bone density scans (DEXA) every 1‑2years for early detection of osteopenia.
- Psychological tools: cognitive‑behavioral therapy (CBT‑E), mindfulness, and, when needed, SSRIs to address co‑occurring depression or anxiety.
Adopting a balanced eating plan, eliminating secretive dieting, and building a supportive network dramatically improve long‑term outcomes.
Key Take‑aways
- Physical damage from bulimia accumulates silently; electrolyte loss and dental erosion are often the first visible signs.
- Long‑term hormonal and bone complications can appear decades later, emphasizing the need for regular medical screening.
- Mental‑health sequelae are intertwined with the body’s physiological stress, making combined treatment essential.
- Recovery is possible at any stage; proactive monitoring can stop further deterioration.
Frequently Asked Questions
Can bulimia cause permanent heart damage?
Yes. Chronic potassium loss weakens the heart muscle, leading to arrhythmias that can become irreversible if left untreated. Regular cardiac monitoring can catch early changes.
How long does it take for dental erosion to become noticeable?
Visible enamel thinning can appear after 6‑12months of frequent vomiting. Early signs include tooth sensitivity and a yellowish tint along the gum line.
Is bone loss from bulimia reversible?
To some extent. Adequate calcium, vitamin D, weight‑bearing exercise, and hormone‑balancing therapy can improve bone density, but severe osteoporosis may remain.
Do electrolyte supplements replace medical labs?
No. Over‑the‑counter supplements can mask symptoms but don’t provide the comprehensive picture that blood work offers. Lab testing is essential for safe management.
What mental‑health therapies work best for long‑term recovery?
Evidence‑based CBT‑E (Cognitive Behavioral Therapy‑Enhanced) combined with mindfulness and, when appropriate, SSRI medication, shows the highest remission rates over a 12‑month period.




11 Comments
sachin shinde
While the article admirably attempts to catalogue the sequelae of bulimia, it suffers from a litany of orthographic oversights that undermine its credibility. For instance, "electrolyte loss can trigger heart rhythm problems" is a tautology; the phrase "heart rhythm problems" is redundant when the preceding clause already mentions "electrolyte loss." Moreover, the inconsistent use of British vs. American spelling (e.g., "behaviour" vs. "behavior") distracts the reader.
One would expect a medical overview to adhere to a tighter editorial standard, especially given the gravity of the subject matter. The omission of citations further erodes trust. In short, the piece could benefit from a rigorous copy‑editing pass before it is presented as an authority.
Additionally, the bullet points alternate between present and past tense, creating a jarring reading experience. Consistency in voice is essential for clarity. Finally, the HTML markup includes stray tags that could break rendering on certain browsers. A thorough review would elevate the article from a decent primer to a professional reference.
Leon Wood
Wow, thanks for the deep dive! This info is gold for anyone battling bulimia and looking for a roadmap to recovery. It’s empowering to see that early intervention can actually stop the damage before it becomes permanent. Keep spreading the word-every person who reads this gets a step closer to healing! 💪
George Embaid
Great points on the presentation, and I’d add that the medical details themselves are spot‑on. The breakdown of electrolyte issues, dental erosion, and bone health gives readers a clear picture of what to monitor. Pairing this with culturally sensitive resources can help reach diverse communities who might otherwise feel excluded from the conversation.
Meg Mackenzie
Reading this article reminded me of the countless whispers that circulate behind closed doors, where the “official” narrative often masks deeper, systemic failures. It’s not just about potassium levels or enamel loss; it’s about a society that silently condones the stigmatization of eating disorders while offering minimal support. The chronic stress described-shifting from shame to anxiety-mirrors the covert surveillance we experience in everyday life, where every bite can feel like a potential betrayal.
Moreover, the suggestion that “regular labs every 3‑6 months” may be a luxury for those lacking health insurance, pushing them further into the shadows. I’ve heard from friends that the very act of seeking help can trigger paranoia about being labeled or monitored, especially when pharmaceutical interventions are involved.
The article’s recommendation for multidisciplinary teams sounds ideal, yet the reality is that many communities lack even a single specialist. This creates a vacuum that is often filled by misinformation, ranging from dubious “detox” teas to fringe theories about hidden agendas.
It’s terrifying to think that a young person could be swayed toward dangerous self‑treatment because the institutional safety nets are so thin. While the emphasis on bone density scans is crucial, one must consider that access to DEXA machines is limited in rural areas, leaving many to guess about their own skeletal health.
The link between hormonal imbalance and fertility is another area where misinformation thrives; some claim it’s a myth, while others warn of irreversible damage. Both extremes ignore the nuanced truth that early, compassionate intervention can indeed mitigate many of these risks.
The article’s thoroughness deserves applause, but we must also advocate for broader policy changes that make these screenings affordable and routine. Only then can we bridge the gap between knowledge and actual, equitable health outcomes.
In short, the piece is a solid foundation, yet the real battle lies in dismantling the barriers that keep people from accessing the care it describes.
Shivaraj Karigoudar
Yo fam, lemme break down the whole thing in layman’s lingo but with a dash of med‑jargon ‘cause we need that cred. When you’re constantly chuggin’ laxatives and purge after binging, you’re basically hijacking your gut’s neuro‑hormonal feedback loops, which can lead to dysmotility and gastroparesis over the long haul. Not to mention the chronic hypokalaemia, which is like a silent assassin for cardiac repolarization – you could end up with torsades de pointes without even feeling the vibe.
Dental erosion? Yeah, that’s just the enamel saying “adios” after years of exposure to gastric acid, and you’ll need crowns or veneers if you don’t intervene. Bone health takes a hit too – low estrogen from disrupted LH/FSH axis means osteopenia can set in faster than a Netflix binge.
So, the TL;DR is: keep tabs on labs, get a dietitian on speed‑dial, and maybe consider a CBT‑E protocol to rewire those maladaptive reward pathways. Stay safe and stay real.
Madeline Leech
Honestly, this whole “dietitian on speed‑dial” talk sounds like another foreign‑imported fad. In our country, we know the real problem is the social decay that pushes people to these extremes. It’s high time we stop glorifying “CBT‑E” and focus on building strong community values that keep our youth grounded.
Barry White Jr
Good info, thanks.
Andrea Rivarola
Appreciate the concise nod, and I’ll add that brevity, while valuable, can sometimes gloss over the intricate biochemistry underlying bulimia’s systemic impact. When potassium homeostasis is repeatedly disrupted, we see alterations in the Na⁺/K⁺‑ATPase pump function, which cascades into mitochondrial inefficiencies, potentially exacerbating fatigue and cognitive fog.
Moreover, the chronic activation of the hypothalamic‑pituitary‑adrenal axis not only affects cortisol levels but also modulates leptin signaling, influencing appetite regulation. It’s fascinating how these endocrine feedback loops intertwine, creating a vicious cycle that sustains the disorder.
That’s why multidisciplinary monitoring, including endocrinology consultations, can be a game‑changer for long‑term prognosis. In sum, while a brief acknowledgment is nice, delving deeper reveals a web of physiological disruptions that merit thorough examination.
Tristan Francis
Bulimia can mess up your heart and teeth. It can also make your bones weak. Getting help early is important.
Keelan Walker
Exactly! 🙌 early check‑ups can catch the heart rhythm issues before they get scary 😱 and a quick dentist visit can save those pearly whites 😁 remember labs every few months keep the electrolytes in check 💊 stay strong 💪
Henry Kim
I find the detailed recommendations helpful, especially the suggestion for regular metabolic panels and DEXA scans. It’s reassuring to see a balanced approach that includes both physical and psychological care without pushing any single treatment avenue.