Emergency Medications: What You Need to Know When Seconds Count
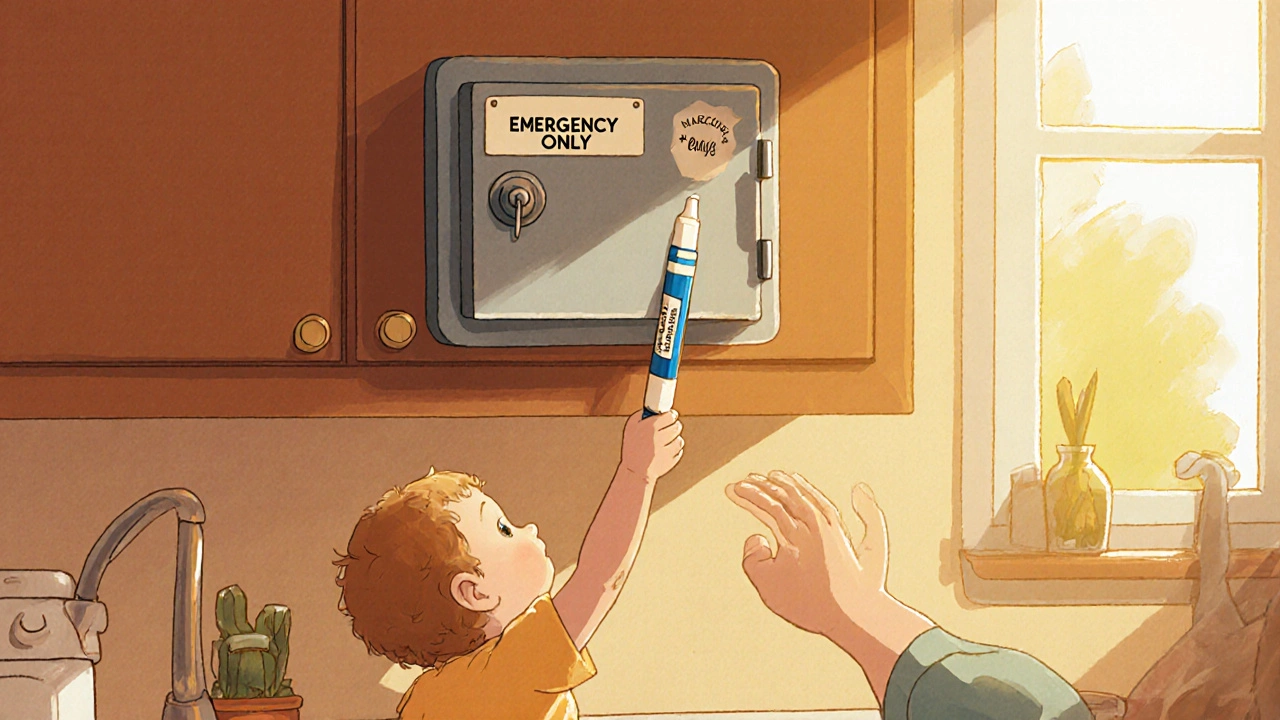
When something goes wrong fast—whether it’s a severe allergic reaction, a heart attack, or an opioid overdose—emergency medications, drugs designed to act quickly in life-threatening situations. Also known as rescue medications, these aren’t for daily use. They’re your last line of defense when time is the only thing you can’t afford to lose. Unlike regular prescriptions, these drugs work in minutes, not days. They don’t cure anything. They buy you time—time to get to the hospital, time for help to arrive, time to breathe again.
Think of epinephrine, the first-line treatment for anaphylaxis. It’s the only thing that can reverse swelling in the throat, drop blood pressure, or shut down a runaway immune response. Without it, death can come in under ten minutes. Then there’s naloxone, a drug that reverses opioid overdoses. It doesn’t feel like magic—but it might as well. A single nasal spray can wake someone up who’s stopped breathing. And nitroglycerin, used for angina and heart attack symptoms. It opens up clogged arteries fast, easing chest pain before the ambulance even turns on its lights. These aren’t just pills or injections. They’re tools that turn panic into action.
But using them right matters more than having them. Too many people keep epinephrine in a drawer, forgetting it expires. Others don’t know how to tell if someone’s having a heart attack versus indigestion. And insulin? It’s not just for diabetics—it’s an emergency drug when blood sugar crashes too low. You don’t need to be a doctor to use these. But you do need to know the signs: hives and trouble breathing? Epinephrine. Blue lips and no response? Naloxone. Crushing chest pain that won’t go away? Nitroglycerin. Slow, shaky, sweating? Give glucose or insulin if you’re trained. These aren’t guesses. They’re protocols backed by real-world outcomes.
The posts below cover what happens when things go wrong—and what to do next. You’ll find guides on how metoclopramide can cause movement disorders if misused, why folic acid is critical with methotrexate, and how grapefruit can turn a safe statin into a danger. You’ll see how warfarin patients find support, how recalls like Valsartan-Hydrochlorothiazide affect your safety, and why therapeutic drug monitoring matters for narrow window drugs. These aren’t abstract discussions. They’re stories of real people who relied on the right drug at the right time—and what happened when they didn’t. This isn’t about being prepared. It’s about being ready when no one else is.