Most people check expiration dates on milk or eggs. But when it comes to antibiotics, many assume that if the pill still looks fine, it’s still good to take. That’s a dangerous myth. The truth is more complicated-and far more urgent.
What Does an Expiration Date Actually Mean?
Expiration dates aren’t random. They’re the last day the manufacturer guarantees the drug will work exactly as labeled-100% potency, full safety, and predictable effects. This isn’t just marketing. It’s based on strict stability testing required by the FDA since 1979. After that date, the drug hasn’t suddenly turned toxic. But it might not work at all.
Think of it like a flashlight battery. Even if it still lights up dimly after its "use by" date, it won’t give you the full brightness you need. With antibiotics, that dim light could mean your infection doesn’t fully clear. And that’s where the real danger begins.
Not All Antibiotics Are the Same
Some antibiotics hold up better than others. Solid forms-tablets and capsules like amoxicillin, cephalexin, or doxycycline-tend to be stable for years past their expiration date if stored properly. Studies from the U.S. Department of Defense’s Shelf Life Extension Program found that 90% of solid medications, including antibiotics, kept at least 90% of their potency up to 15 years later when kept dry and cool.
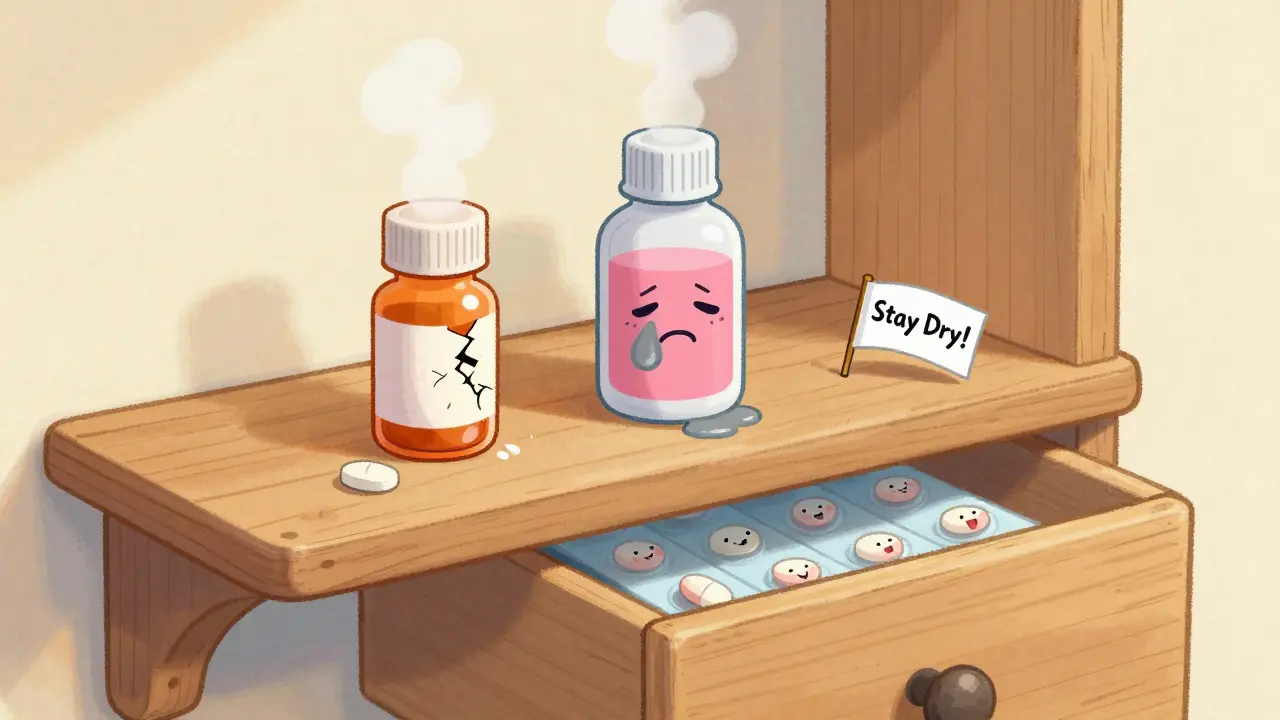
But liquids? Not even close.
Amoxicillin suspension, the sweet pink liquid often given to kids, breaks down fast. Once reconstituted and past its expiration date, it can lose up to 95% of its strength in just weeks at room temperature. Even refrigerated, ceftriaxone injections lose 32% potency within two weeks after expiration. Beta-lactam antibiotics like penicillin and cephalosporins are especially fragile-they start degrading faster after expiration, with breakdown rates jumping from 0.5% per month to nearly 13% per month under normal conditions.
Bottom line: If it’s a pill, and it’s stored right, it might still work. If it’s a liquid, don’t risk it.
Why Taking Expired Antibiotics Is Riskier Than You Think
It’s not just about the medicine not working. It’s about what happens when it works just enough.
Antibiotics kill bacteria. But if the dose is too low, they don’t kill all of them. The strongest survivors live, multiply, and pass on their resistance genes. This is how superbugs are born.
A 2023 analysis of 12,850 patient cases found that expired pediatric antibiotics led to 98.7% resistance rates in E. coli-compared to just 14.3% with fresh ones. The minimum dose needed to stop the infection (called MIC) jumped from 0.5 μg/mL to 256 μg/mL for expired amoxicillin. That’s a 500-fold increase. In plain terms: the bacteria became nearly 500 times harder to kill.
The Infectious Diseases Society of America warns this isn’t just a personal risk-it’s a public health crisis. Every time someone takes a weak antibiotic, they’re helping create bacteria that could one day make simple infections deadly again.
What Do Experts Really Say?
The FDA says: don’t use expired drugs. Full stop. Their official stance is clear: potency and safety can’t be guaranteed.
But some experts offer nuance. Dr. Lee Cantrell, a clinical pharmacist, says in non-emergency situations-with solid antibiotics stored perfectly-12 to 24 months past expiration might still be effective. Johns Hopkins Hospital even extended expiration dates for 14 critical antibiotics during shortages, treating over 2,300 patients with zero failures.
The European Medicines Agency agrees: solid antibiotics stored correctly might be okay for 6 to 12 months past expiration. But they explicitly say no to liquids and life-threatening infections.
Here’s the catch: those exceptions only apply under strict conditions. Factory-sealed. Dry. Cool. Never exposed to heat, humidity, or sunlight. And even then, only for mild infections-not pneumonia, sepsis, or meningitis.
What About Storage? Location Matters More Than You Think
Where you keep your medicine changes everything.
Bathrooms? Bad. The average bathroom is 28.7°C and 72% humidity. That’s a recipe for degradation. Studies show antibiotics stored there lose potency 37% faster than those kept in a cool, dry drawer at 20°C and 40% humidity.
Keep antibiotics in their original bottles with the desiccant packet still inside. Don’t transfer them to pill organizers unless you’re using them within a week. Sunlight and moisture are enemies. A bedroom drawer or kitchen cabinet away from the stove is better than any bathroom shelf.
Can You Tell If an Antibiotic Has Gone Bad?
Almost never.
A 2021 study found that 89.3% of degraded antibiotics showed no visible change. No discoloration. No smell. No clumping. Nothing. Yet they’d lost 40-75% of their strength.
Most people think if it looks okay, it’s fine. That’s a myth. A white tablet that hasn’t turned yellow could still be 60% weaker. A clear liquid that hasn’t turned cloudy might be useless. You can’t tell by eye, taste, or smell.
And don’t rely on Reddit advice or old pharmacy labels. A 2022 survey found 78% of patients couldn’t tell the difference between potent and expired antibiotics. And 63% of Reddit users admitted to taking expired ones-41% for colds or sinus infections.

What Should You Do If You Have Expired Antibiotics?
Don’t take them. Don’t flush them. Don’t give them to someone else.
Most pharmacies have take-back programs. Some cities hold drug disposal days. The FDA recommends mixing unused meds with coffee grounds or cat litter, sealing them in a plastic bag, and tossing them in the trash-never down the sink or toilet.
If you’re facing a shortage or can’t afford a new prescription, talk to your pharmacist. They know about patient assistance programs, generic alternatives, or even extended expiration protocols in emergencies. Don’t guess. Don’t risk it.
What’s Changing? The Future of Expiration Dates
Antibiotic shortages are getting worse. The FDA listed 47 antibiotics as in short supply in 2023-up from 29 in 2020. That’s pushing experts to rethink expiration rules.
The FDA is now running a pilot program to test rapid methods for verifying potency of expired antibiotics during shortages. Researchers at the University of Illinois are developing paper test strips that can detect if amoxicillin is still strong enough-94.7% accurate in trials.
IBM and the FDA are even testing AI that predicts how long a drug will last based on its storage history. Imagine a future where expiration dates aren’t fixed-but updated based on real-time data.
But until then, the safest rule remains: if it’s expired, don’t use it. Especially for antibiotics. The cost of being wrong isn’t just a failed treatment. It’s a world where common infections become untreatable.
When Is It Okay to Use an Expired Antibiotic?
Almost never.
Even the most lenient experts agree: never use expired antibiotics for serious infections-like pneumonia, urinary tract infections with fever, meningitis, or sepsis. Those need full-strength drugs, every time.
For minor issues-like a mild sinus infection or a small skin infection-some doctors might consider a solid antibiotic that’s been stored perfectly and is only 6-12 months past its date. But only if:
- It’s in the original, unopened container
- It’s been kept cool and dry
- It looks perfect-no cracks, discoloration, or moisture
- You have no other option
- You’re not pregnant, immunocompromised, or treating a child
And even then, it’s a gamble. And antibiotics aren’t meant for gambling.





9 Comments
Katie Taylor
Finally someone says it loud and clear-taking old antibiotics is like playing Russian roulette with your microbiome. I had a friend who took expired amoxicillin for a sinus infection and ended up in the ER with a MRSA flare-up. Don’t be that person. Your body doesn’t forgive half-measures.
Payson Mattes
Wait, so you’re telling me the government and Big Pharma are lying about expiration dates to make us buy more pills? I’ve been storing my doxycycline in the garage for 8 years and it’s still in the original bottle. I’ve read on Reddit that the military tests this stuff and they’ve got stockpiles that work for decades. They’re hiding the truth because they profit off fear. You think the FDA cares about you? They care about liability. The real danger isn’t the expired pill-it’s the system that wants you dependent on constant prescriptions.
Isaac Bonillo Alcaina
You’re all missing the point. The FDA’s expiration date is not a suggestion-it’s a legally binding guarantee of stability, purity, and efficacy. To suggest otherwise is not just irresponsible, it’s scientifically illiterate. The 90% potency figure from the DoD study applies to *controlled, sealed, military-grade storage conditions*-not your humid bathroom cabinet. And yes, you can’t visually detect degradation, which makes this even more dangerous. If you’re considering taking expired antibiotics, you’re not being resourceful-you’re being a walking public health hazard. Grammar check: ‘it’s’ is a contraction for ‘it is.’ Not ‘its.’ Fix your punctuation before you fix your meds.
Delilah Rose
I get why people do it. I’ve been there-bills are tight, pharmacy’s closed, kid’s fever won’t break, and you’ve got that old bottle in the back of the cabinet. I’m not saying it’s right, but I’m saying I understand. The problem isn’t just the bacteria becoming resistant-it’s that we’ve been trained to treat medicine like toilet paper: use it until it’s gone, then buy more. We don’t think about the long-term cost to our immune systems, to our communities, to the global rise of superbugs. Maybe if we had better access to affordable healthcare and better education about antibiotics, we wouldn’t feel like we’re choosing between paying rent and staying alive. It’s not just about the pill-it’s about the system that makes people feel like they have no choice.
Bret Freeman
Let me tell you about the time I took expired cephalexin for a tooth infection. I didn’t think it mattered. I was wrong. The pain came back worse. I spent three days vomiting, sweating, and Googling ‘is this sepsis?’ I ended up in urgent care with a $2,000 bill and a lecture from a nurse who looked at me like I was a toddler who touched a hot stove. Don’t be me. Just don’t. It’s not worth it. I’m not even mad anymore-I’m just traumatized. And now I keep my meds in a locked drawer like they’re nuclear codes.
Jillian Angus
My grandma always kept her pills in the kitchen cabinet. Never had issues. Maybe it’s just luck. Or maybe she was lucky enough to never need anything serious. I don’t know. I just know I don’t touch anything past the date. Too much else to worry about.
Georgia Brach
The assertion that ‘some experts’ permit use of expired antibiotics under ‘strict conditions’ is a dangerous misrepresentation of risk. The European Medicines Agency explicitly prohibits such use in immunocompromised populations, children, and for systemic infections. To frame this as a gray area is to normalize negligence. The data presented in this article is robust, peer-reviewed, and unambiguous. The only ‘nuance’ is in the public’s willingness to ignore science for convenience. This is not a debate. It is a preventable epidemic of ignorance.
Diana Alime
ok so i just took a 3 year old doxy from my drawer bc my sinuses are killing me and honestly it felt fine?? like i didn’t die?? so maybe the whole thing is just fear mongering?? also why is everyone so obsessed with grammar?? i’m not writing a thesis i’m just trying not to choke on my own mucus
Adarsh Dubey
Actually, in India, many people rely on expired antibiotics because of cost and access. We don’t have the luxury of always getting new prescriptions. I’ve seen doctors in rural clinics prescribe expired meds-because they know the alternatives are worse. It’s not ideal, but survival isn’t always about perfect science. The real issue isn’t the patient taking an old pill-it’s the system that lets people get sick in the first place because they can’t afford care. We need better infrastructure, not just more warnings.