Quercetin Medication Risk Calculator
Check Your Risk
Risk Assessment
Disclaimer: This tool is for educational purposes only. It does not replace professional medical advice. Always consult your healthcare provider before changing medications or supplements.
Most people take quercetin supplements for its anti-inflammatory properties, thinking it’s just another natural antioxidant. But if you’re also on prescription meds-especially blood thinners, heart drugs, or cancer treatments-this supplement could be quietly changing how your body processes your medication. And you might not even know it.
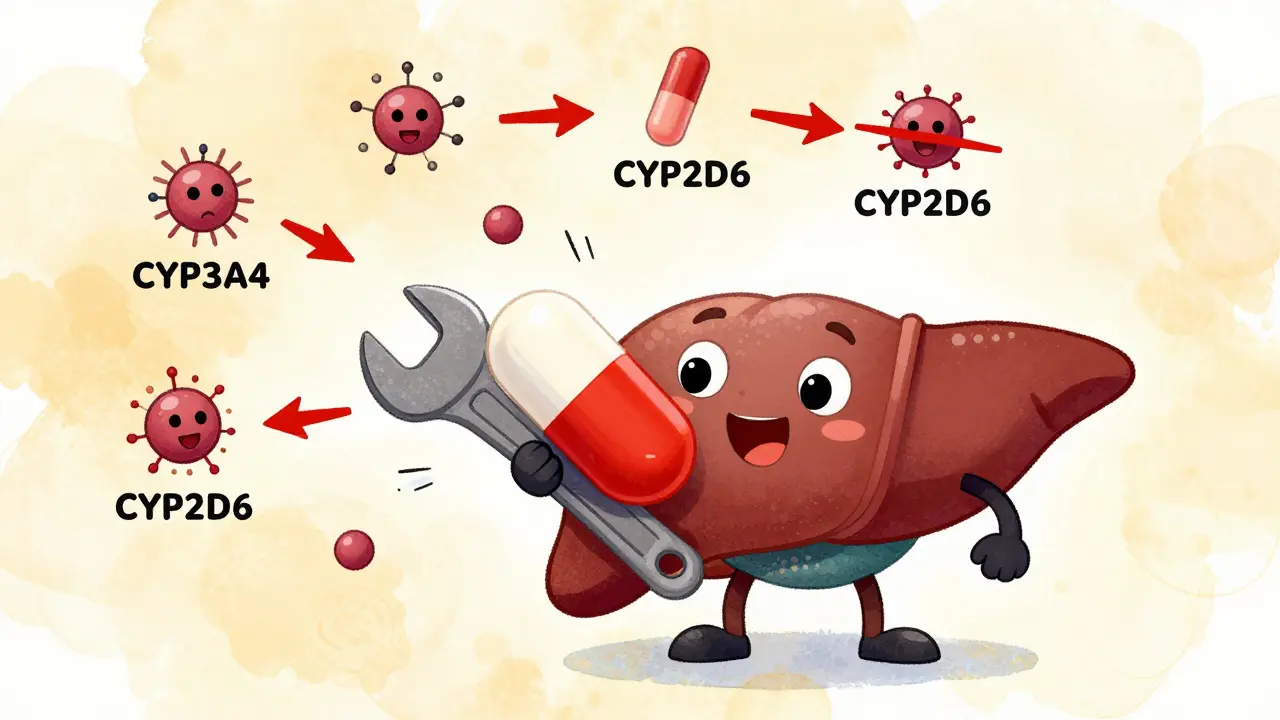
What Quercetin Actually Does to Your Liver
Quercetin isn’t just a plant compound. At high doses, it acts like a molecular wrench thrown into your body’s drug-processing system. It targets enzymes in your liver and gut called cytochrome P450 (CYP), especially CYP3A4, CYP2D6, and CYP2C19. These enzymes are responsible for breaking down more than half of all prescription drugs. When quercetin blocks them, your meds don’t get broken down as quickly. That means they build up in your bloodstream-sometimes way beyond safe levels.
Studies show quercetin can reduce the metabolism of drugs like abemaciclib (a cancer drug) by 25-35%, and acenocoumarol (a blood thinner) by 30-45%. In lab tests, a concentration of just 10 micromolars of quercetin blocked up to 85% of CYP2D6 activity. That’s not a small effect. It’s the same level of inhibition seen with some strong prescription inhibitors.
Which Medications Are Most at Risk?
Not all drugs are affected equally. The danger is highest with medications that have a narrow therapeutic index-meaning the difference between a helpful dose and a toxic one is tiny. Here are the top categories at risk:
- Blood thinners: Warfarin, acenocoumarol, and even newer ones like apixaban and rivaroxaban. Quercetin can raise INR levels by 0.8-1.5 points, increasing bleeding risk.
- Immunosuppressants: Cyclosporine and tacrolimus. One study found quercetin could raise cyclosporine levels by 30-50%, putting transplant patients at risk of kidney damage.
- Heart medications: Diltiazem, verapamil, and some beta-blockers metabolized by CYP3A4 or CYP2D6.
- Cancer drugs: Abemaciclib, erlotinib, and other tyrosine kinase inhibitors. Higher drug levels can cause severe side effects like diarrhea, low blood counts, or liver toxicity.
- Antidepressants and anti-anxiety meds: SSRIs like sertraline, and tricyclics like amitriptyline, which rely heavily on CYP2D6.
- Pain relievers: Acetaminophen (Tylenol) levels can rise 20-30%, raising liver strain risk, especially in people who drink alcohol or have existing liver issues.
Even if you’re not on one of these drugs now, you might be in the future. Many people start taking quercetin for general wellness, then later get prescribed a new medication. The interaction doesn’t always show up right away-it can sneak in months later.
Why Food Isn’t the Problem-But Supplements Are
You can eat apples, onions, capers, and broccoli all day and not worry. The quercetin in food is bound to sugars (called glycosides), which your body absorbs slowly and converts into less active forms. But supplements? They deliver pure, unbound quercetin-often 500 mg or more per pill. That’s 100 to 1,000 times more than you’d get from diet.
One study found quercetin glycosides (like rutin) are only 30-40% as potent as the aglycone form found in pills. So yes, your daily salad is fine. But if you’re popping a capsule labeled “500 mg quercetin,” you’re introducing a pharmacologically active compound that behaves like a drug.

Who’s Most at Risk?
It’s not just about what you take-it’s about who you are.
- People over 65: Metabolism slows with age. Older adults clear quercetin 25-40% slower, so it lingers longer and builds up.
- People on multiple medications: If you’re taking five or more prescriptions, the chance of overlapping metabolic pathways increases. Quercetin doesn’t just affect one enzyme-it hits several at once.
- People with liver or kidney disease: Your body already struggles to clear drugs. Adding quercetin makes it worse.
- Transplant recipients: Even small changes in cyclosporine or tacrolimus levels can trigger rejection or toxicity.
And here’s the scary part: most people don’t tell their doctors they’re taking supplements. A 2021 survey found that 62% of quercetin users never mentioned it to their healthcare provider. That’s like taking a new pill without telling your doctor.
What the Experts Say
The European Food Safety Authority (EFSA) warned in 2018 that doses above 1,000 mg/day of quercetin “pose potential concerns for drug interactions.” The FDA listed quercetin as a “dietary supplement of concern” in its 2020 draft guidance. The American Society of Health-System Pharmacists (ASHP) says to avoid quercetin entirely if you’re on direct oral anticoagulants (DOACs).
And it’s not just theory. Between 2015 and 2022, the FDA received 147 reports of possible quercetin-drug interactions. That’s just the tip of the iceberg. Experts estimate fewer than 5% of these events get reported. So for every case they know about, there are 20 more going unnoticed.

What You Can Do
If you’re taking quercetin supplements and any prescription meds, here’s what to do:
- Stop taking quercetin for now. Especially if you’re on blood thinners, cancer drugs, or immunosuppressants.
- Talk to your pharmacist. They can check your full med list and flag interactions you might miss. Bring your supplement bottle with you.
- If you must take it, keep the dose under 500 mg/day. And never exceed 1,000 mg.
- Separate timing. Take your medication and quercetin at least 4-6 hours apart. This can reduce interaction risk by 30-50%.
- Watch for symptoms. Unusual bruising, dizziness, nausea, confusion, or muscle pain could signal drug buildup. Get checked immediately.
Some people swear quercetin helps with allergies or fatigue. But if it’s putting your other meds at risk, the trade-off isn’t worth it. There are safer alternatives for inflammation-like omega-3s, curcumin (with caution), or even just walking daily.
The Bigger Picture
The supplement industry is booming. Global sales of quercetin hit $387 million in 2022. Over 18 million Americans take it. And almost half of them are taking more than 500 mg a day. Yet there’s no regulation forcing manufacturers to warn about drug interactions.
The FDA has issued 17 warning letters to quercetin brands for making false health claims. A new rule proposed in 2024 might finally require warning labels on high-risk supplements. But until then, the burden is on you.
This isn’t about fear. It’s about awareness. Natural doesn’t mean safe. And just because something is sold as a supplement doesn’t mean it’s harmless. When it comes to your meds, you need to treat quercetin like a drug-because in your body, that’s exactly what it becomes.
Can I take quercetin with warfarin?
No. Quercetin can increase warfarin levels in your blood, raising your INR and significantly increasing your risk of bleeding. Even small increases in INR can lead to dangerous bruising, nosebleeds, or internal bleeding. If you’re on warfarin, avoid quercetin supplements entirely. Talk to your doctor about safer anti-inflammatory options.
Is quercetin safe with statins like atorvastatin?
It’s risky. Atorvastatin is metabolized by CYP3A4, which quercetin strongly inhibits. This can cause statin levels to rise, increasing the chance of muscle pain, weakness, or a rare but serious condition called rhabdomyolysis. If you’re on a statin, avoid high-dose quercetin. If you must use it, keep the dose under 250 mg and monitor for muscle symptoms.
How long does quercetin stay in your system?
Quercetin has a half-life of about 11-28 hours in healthy adults, but it can linger longer in older people or those with liver issues. Its metabolites can stay active for up to 48 hours. That means even if you take quercetin in the morning, it can still affect how your evening medication is processed. For safety, separate it from meds by at least 6 hours.
Does grapefruit juice have the same effect?
Grapefruit juice is a stronger inhibitor of CYP3A4 than quercetin, but quercetin affects more enzymes overall. Grapefruit mainly hits CYP3A4, while quercetin also strongly blocks CYP2D6 and CYP2C19. So while grapefruit is notorious, quercetin is broader and harder to avoid-especially since it’s in pills you might not even think of as dangerous.
Are there any supplements that are safer alternatives?
Yes. For inflammation or immune support, consider omega-3 fatty acids (fish oil), vitamin D, or curcumin (turmeric extract)-but even curcumin can interact with some drugs, so check with your pharmacist. The safest options are lifestyle-based: regular movement, sleep, and reducing processed foods. These don’t interfere with meds and offer real, proven benefits.



11 Comments
Alvin Bregman
Man i just started taking this quercetin thing for my allergies and now im reading this like oh crap
Robert Way
so wait you saying my daily capslue is as bad as grapefruit juice?? i thought that was the only thing to watch out for
Sarah Triphahn
people are so naive thinking natural means safe. its like saying a rock is safe because its not plastic. dumb. this is why we have so many hospital visits from supplements
Vicky Zhang
oh my gosh i had no idea. i take this for my fatigue and my blood pressure med and now im terrified. i just called my pharmacist and they said to stop immediately. thank you for posting this. i feel like i almost killed myself with good intentions
Allison Deming
It is both irresponsible and alarming that the supplement industry operates without any meaningful regulatory oversight. Consumers are being misled into believing that these compounds are benign when, in fact, they possess pharmacological potency comparable to prescription medications. This is not a matter of personal choice-it is a public health failure.
Susie Deer
usa lets go we dont need no regulation. if you wanna take pills then take em. its your life not mine
says haze
It’s fascinating how society romanticizes plant compounds while demonizing pharmaceuticals. Yet the biochemical reality is identical-molecular interactions don’t care about labels. Quercetin is a CYP inhibitor. End of story. The myth of natural superiority is just cognitive dissonance dressed up as wellness.
shiv singh
you people are so scared of everything. i take quercetin and my cancer med and i feel better than ever. you just want to control us with fear. big pharma hates this stuff because its cheap and natural. you all are sheep
TooAfraid ToSay
wait so you mean to tell me the guy who sells this at the farmers market is more dangerous than my oncologist? i think im gonna double my dose now just to prove a point
Dylan Livingston
how do you survive in this world if you dont even know your own liver is a fragile little flower? i mean really. you take a pill you think is harmless and then wonder why you’re dizzy and bruising. it’s not rocket science. it’s basic biology. and yet here we are.
Andrew Freeman
lol i take 1000mg a day with my statin and im fine. this article is just fearmongering. next theyll say water is dangerous if you drink it with pills