Most people will deal with low back pain at some point in their life. It’s not rare. It’s not unusual. In fact, 80% of adults will experience it. But here’s the thing: 97% of those cases aren’t dangerous. They’re just annoying, stiff, and frustrating. The real problem? Too many people panic, rush to get an MRI, or assume something terrible is wrong-when they don’t need to.
So how do you know if your back pain is just a bad muscle strain or something serious? And what should you actually do about it? Let’s cut through the noise.
What Are Red Flags, and Why Do They Matter?
Red flags aren’t scary symptoms. They’re warning signs that something more serious might be going on. Think of them like a check engine light in your car-not every flicker means a blown engine, but ignoring it could cost you.
The big four red flags to watch for are:
- Malignancy: A history of cancer, especially if it was breast, lung, prostate, or kidney cancer. Unintentional weight loss (more than 5% of your body weight in 6 months) is another major red flag.
- Fracture: Especially if you’ve had a major fall, car crash, or if you’re on long-term steroids or have osteoporosis. Even a minor fall can break a bone if your bones are weak.
- Cauda equina syndrome: This is rare but dangerous. Symptoms include losing control of your bladder or bowels, numbness in your saddle area (inner thighs, genitals, anus), or trouble peeing (especially if you’re holding more than 200cc of urine after trying to go).
- Infection: Fever, IV drug use, or severe pain when someone taps on your spine. If you’ve had recent surgery or a skin infection, this becomes more likely.
Here’s what’s not a red flag: age over 50, mild numbness in your leg, or pain that gets worse when you sit. These are common-and normal-parts of back pain. Yet, a 2022 survey found that nearly 70% of doctors still wrongly think age alone means you need an X-ray or MRI. That’s outdated thinking.
When Should You Get Imaging (X-ray, MRI, CT)?
Most of the time? You shouldn’t. Not right away.
Major guidelines from the American College of Radiology, the American College of Physicians, and Canada’s family doctors all agree: if you have low back pain for less than 4 weeks, with no red flags, no imaging is needed. Not an X-ray. Not an MRI. Not even an ultrasound.
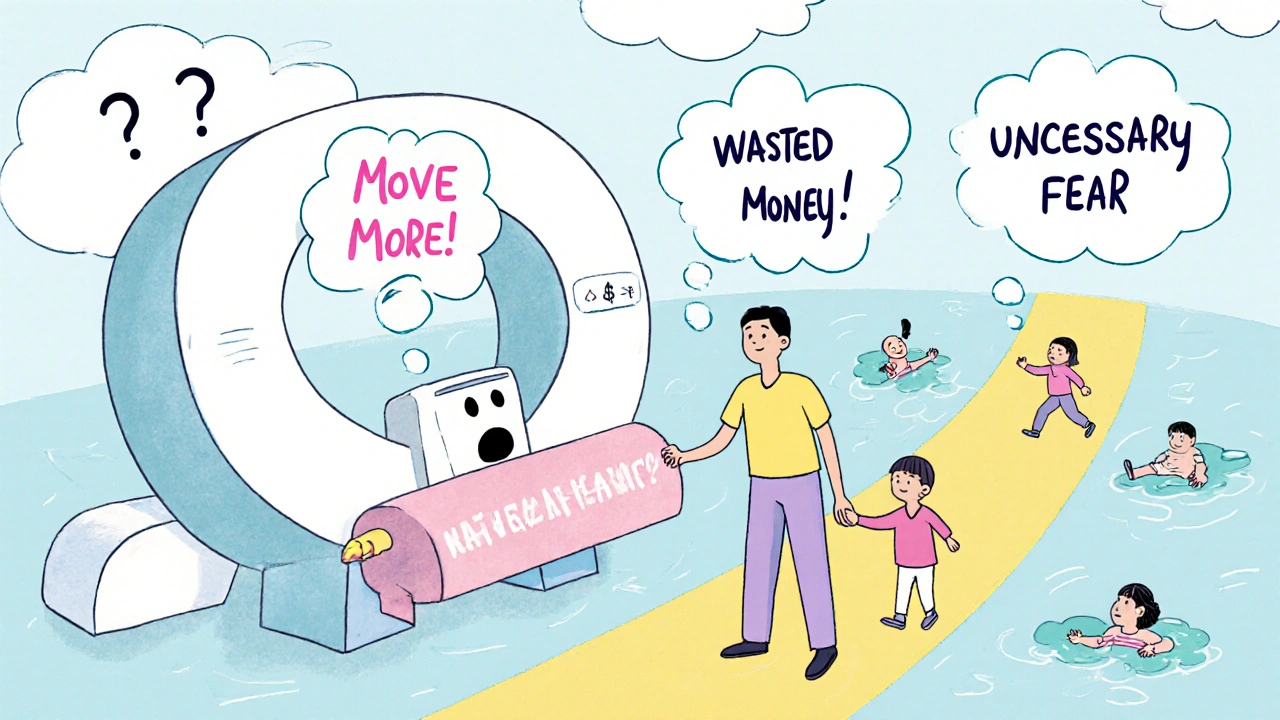
Why? Because imaging rarely shows the real cause of pain in these cases. You might see a bulging disc or arthritis on the scan-but those show up in people with no pain at all. Finding them doesn’t help. It just scares you.
Imaging is only appropriate when:
- Red flags are present (especially for cauda equina or suspected infection)
- You have progressive neurological symptoms (like worsening leg weakness or numbness)
- Your pain hasn’t improved after 6-12 weeks of conservative care
For suspected cancer or spinal infection, MRI without contrast is the gold standard. For fractures, especially in older adults, a CT scan might be better. But again-only if the red flags are there.
And here’s the kicker: getting an X-ray for routine back pain doesn’t improve outcomes. It just adds cost. In the U.S. alone, unnecessary imaging for back pain costs about $3 billion a year. That’s money wasted on scans that don’t help-and often lead to more tests, more anxiety, and even unnecessary surgery.
Exercise Therapy: The Most Proven Treatment You’re Not Doing
If you’ve been told to rest, stay off your feet, or wait for the pain to go away on its own-you’ve been given bad advice.
Strong evidence from 97 clinical trials involving nearly 20,000 people shows that exercise therapy reduces pain and improves function better than any pill, injection, or passive treatment like massage or ultrasound. The Cochrane Review found people who exercised had, on average, a 6.6-point improvement on a 100-point pain scale compared to those who did nothing. That’s not minor. That’s meaningful.
Not all exercises are equal. Here’s what actually works:
- Motor control exercises: These teach your deep core muscles (like transverse abdominis and multifidus) to fire properly. Think gentle pelvic tilts, dead bugs, and bird-dogs. Effect size: 0.61.
- Graded activity: Slowly increasing your movement and activity level-even if you’re in pain. This breaks the fear-avoidance cycle. Effect size: 0.52.
- Combined programs: Mixing strength, aerobic work, and flexibility. Walking, swimming, cycling, and bodyweight squats all count. Effect size: 0.58.
You don’t need a gym. You don’t need expensive equipment. You need consistency.
The American Physical Therapy Association recommends:
- 2-3 supervised sessions per week for the first 4-6 weeks
- Progress to a home program after that
- Continue for at least 8-12 weeks
Intensity matters. Start at 40-60% of your max effort for strengthening. Work up to 70-85% over time. For cardio, aim for 60-80% of your max heart rate for 20-30 minutes, 3-5 days a week.
And yes, it hurts at first. That’s normal. But if pain shoots down your leg, or you feel numbness or tingling that doesn’t go away, stop and see a professional.
Why So Many People Get It Wrong
Doctors are busy. Patients are anxious. Insurance pushes for quick fixes. The result? A system that over-tests and under-treats.
One study found doctors spend just 12.7 minutes per back pain visit. The recommended time? 18-22 minutes. That’s not enough to properly screen for red flags, explain why imaging isn’t needed, or teach someone how to move safely.
Many patients are told, “It’s just a strain,” and then left alone with no plan. Others are sent for scans that show nothing-and then told, “We don’t know what’s wrong.” That’s not helpful. It’s confusing.
What works better? Tools like the Red Flag Decision Tool, which helps providers assess risk step-by-step: Is there trauma? Weight loss? Bladder issues? Then decide: urgent, possible, or unlikely. A 2021 trial showed this tool cut unnecessary imaging by 28%.
And it’s not just about avoiding scans. It’s about empowering people to move again.
What You Should Do Right Now
Here’s your simple action plan:
- Check for red flags. Do you have any of the big four? If yes-see a doctor immediately. Don’t wait.
- If no red flags, stay active. Walk daily. Avoid bed rest. Move within your pain limits.
- Start simple exercises. Try 10 minutes a day of pelvic tilts, glute bridges, and walking. Do this for 2 weeks.
- Don’t get an X-ray or MRI unless your pain lasts longer than 6-8 weeks or red flags appear.
- Seek a physical therapist if you’re unsure how to move safely. They’ll teach you what to do-not just what not to do.
Back pain isn’t a disease. It’s a signal. And most of the time, the best medicine is movement-not a machine.
What’s Changing in the Field
Guidelines are evolving. The UK’s NICE guidelines no longer list “age over 55” as a red flag. Why? Because research shows age alone doesn’t predict serious problems. That’s progress.
AI is starting to help. A 2022 study showed an AI tool improved red flag detection from 73% to 89% accuracy. That means fewer missed cases and fewer false alarms.
And there’s new funding-like the SPINE Act of 2022-which is investing $15 million into finding biomarkers that can tell us who’s truly at risk for serious spine conditions. That could one day replace guesswork with real science.
But for now? The best tools you have are knowledge and movement.
Is low back pain always a sign of something serious?
No. In fact, 97% of low back pain cases are caused by simple muscle strains, joint stiffness, or poor movement patterns-not serious disease. Only 1-2% involve conditions like cancer, infection, or nerve damage. Most cases improve with time and movement.
Should I get an MRI if my back pain won’t go away?
Not necessarily. If your pain has lasted more than 6-8 weeks but you have no red flags, an MRI still won’t change your treatment plan in most cases. Imaging often shows changes that aren’t causing pain. Focus first on exercise, activity, and seeing a physical therapist. Only consider imaging if symptoms worsen or red flags appear.
Can exercise make my back pain worse?
It can feel worse at first, but it shouldn’t make your pain worse long-term. If you feel sharp, shooting pain down your leg, numbness, or loss of bladder control, stop and seek help. Mild discomfort during movement is normal. Pain that lasts more than a few hours after exercise may mean you’re doing too much too soon. Start slow and build up.
What’s the best type of exercise for low back pain?
Motor control exercises (like pelvic tilts and dead bugs), graded activity (gradually increasing daily movement), and combined programs (walking, swimming, strength training) have the strongest evidence. You don’t need fancy machines. Consistency matters more than intensity. Aim for 20-30 minutes, 3-5 days a week.
How long should I do exercise therapy before seeing results?
Most people start feeling better in 2-4 weeks, but full benefits take 8-12 weeks. The key is sticking with it. Studies show that if you stop exercising before 8 weeks, you’re unlikely to keep the gains. Think of it like brushing your teeth-regular habits create lasting results.
Are painkillers or injections better than exercise?
Painkillers and injections might give short-term relief, but they don’t fix the problem. Exercise improves strength, movement, and long-term pain control. A 2020 Cochrane Review found exercise was more effective than medication at 6-12 months. Injections may help in specific cases, but they’re not a substitute for movement.
Final Thought: Move Like Your Life Depends On It-Because It Does
Low back pain isn’t a life sentence. It’s a chance to learn how your body moves-and how to protect it. The real enemy isn’t your spine. It’s inactivity. Fear. And the myth that pain always means damage.
Red flags are rare. Imaging is overused. And exercise? It’s the most powerful, cheapest, and safest treatment you’ve already got access to.
Get moving. Stay curious. And don’t let a scan define your health.





10 Comments
Kartik Singhal
Look, I get it-exercise is ‘the answer’-but have you ever tried moving when your spine feels like it’s been stapled shut? 😒 The ‘just walk more’ advice is what you give people who haven’t spent 3 years in physical therapy. I’ve done all the bird-dogs. I’ve dead-bugged till I cried. Still got the herniated disc. No magic moves. Just bad luck and a broken spine.
Sandi Moon
How convenient that the medical-industrial complex suddenly ‘discovers’ exercise works-after decades of pushing MRIs, injections, and opioids. The real red flag? The fact that this article reads like a pharmaceutical lobby’s PR draft. Who funds the ‘Cochrane Review’? Who profits when you skip the scan? The system isn’t broken-it’s designed to keep you docile, dependent, and paying for unnecessary interventions. 🕵️♂️🩺
Logan Romine
So let me get this straight: pain = bad, but movement = good, unless movement hurts… then it’s ‘normal discomfort’? 🤔
Dear universe, why must everything be a paradox? If I’m supposed to move like my life depends on it, why does my spine scream like I’m being dragged through a meat grinder? Is this stoicism or self-harm? I’m confused. And also, my cat just stared at me like I’m the problem.
Chris Vere
The body is not a machine to be fixed but a system to be understood. The modern approach treats pain as an error to be erased rather than a signal to be interpreted. Exercise is not a cure but a dialogue. Consistency is not a suggestion but a discipline. The real cost is not the MRI but the silence we keep when we stop listening to our own bodies. We are taught to fear movement because we were never taught how to move with awareness. This is not medicine. This is awakening.
Pravin Manani
Motor control exercises have a standardized effect size of 0.61 in RCTs-this is clinically significant and aligns with neuromotor re-education paradigms. The transverse abdominis and multifidus are key stabilizers, and their delayed recruitment in chronic LBP is well-documented in EMG studies. Graded exposure protocols reduce fear-avoidance behaviors via habituation and cortical recalibration. However, adherence remains the primary confounder-70% of patients discontinue home programs by week 6. We need better behavioral scaffolding.
Mark Kahn
You got this. Seriously. I’ve seen so many people think they’re broken because their back hurts-but you’re not. You’re just out of practice. Start with 5 minutes of walking today. That’s it. No pressure. No goals. Just move. And tomorrow? Maybe 6 minutes. You don’t need to be perfect. You just need to show up. I believe in you. 💪❤️
Leo Tamisch
Oh wow. Another ‘move more’ manifesto. How original. 🙄
Let me guess-the author also thinks yoga fixes capitalism and that ‘positive vibes’ cure osteoporosis. Look, I get it. Exercise is cheaper than scans. But your ‘simple plan’ ignores that some of us have nerve damage, degenerative disc disease, or a spine that looks like a twisted pretzel on MRI. No amount of pelvic tilts fixes structural reality. This isn’t empowerment-it’s toxic positivity wrapped in a Cochrane review.
Daisy L
OH MY GOD YES!! I’ve been screaming this from the rooftops!! Why do we keep letting Big Pharma and Big Radiology gaslight us?! My neighbor got an MRI for ‘a little back twinge’ and ended up with FIVE surgeries and a $120K bill!! Meanwhile, I just started walking around the block every day-and my pain? GONE. No pills. No needles. No ‘spinal decompression’ scams. Just me, my sneakers, and a stubborn refusal to be scared by a scan. America, wake up!! 🇺🇸🔥
Anne Nylander
ok so i just started doing the pelvic tilts and i think i did them wrong?? my back hurts more now?? but i’m trying!! i’m not giving up!! maybe i need a PT?? anyone know a good one in nyc??
Sammy Williams
Anne, I feel you. I did the same thing-thought I was doing bird-dogs right, ended up crying on the floor. Found a PT who told me to just breathe through it and not push. Took me 3 weeks to realize I was holding my breath the whole time. You’re not failing. You’re learning. Keep going. And yeah, PTs are worth their weight in gold. I’ll DM you one I love.