Mesalamine and IBD: Real Results and Practical Advice (September 2024)
Could one medication really calm chronic gut inflammation enough to get your life back? For many people with ulcerative colitis and some forms of IBD, mesalamine has done exactly that. This archive looks at a September 2024 post that shares real patient stories, how the drug works, what to watch for, and practical tips you can use right away.
How mesalamine works and what to expect
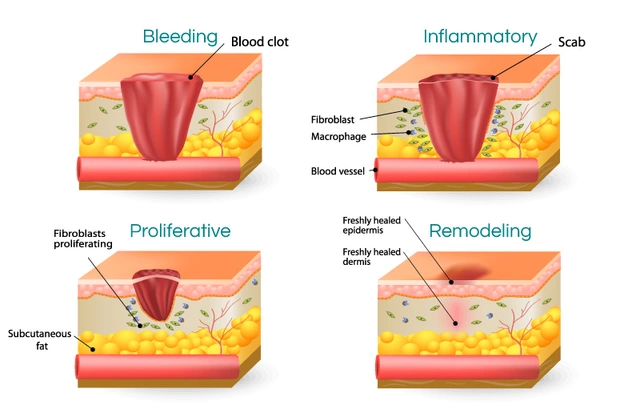
Mesalamine is an anti-inflammatory that targets the lining of the colon. It’s often used for mild-to-moderate ulcerative colitis and for maintenance to prevent flares. Clinical trials and patient registries show it reduces symptoms like bleeding and frequent bowel movements and lowers flare rates when taken correctly.
Expect improvement over weeks, not days. Some people notice symptom relief in two weeks; others need six to eight weeks. Topical forms (suppositories or enemas) work faster for rectal symptoms, while oral delayed-release tablets treat inflammation higher in the colon. If your symptoms don’t change in a couple months, talk to your doctor—dose adjustments or a different treatment might be needed.
Real patient experience and outcomes
One reader story published in September described a patient who went from constant urgency and bleeding to months without a flare after starting mesalamine suppositories combined with oral tablets. Another person reported fewer side effects than predicted and a return to normal activities like work and travel. These stories show two things: adherence matters, and combining oral and topical forms can help when symptoms are limited to the rectum or lower colon.
Side effects are usually mild—headache, nausea, or mild abdominal pain. Rarely, mesalamine can affect the kidneys or cause allergic reactions. Most specialists check kidney function before starting and during treatment, especially for older adults or those on other medications that affect the kidneys.
Practical tips: follow the prescription exactly. Don’t crush or chew delayed-release tablets. If you’re given both oral and rectal forms, use them as instructed—many patients see better control when both are used together. Keep a symptom diary: record bowel frequency, bleeding, and medications. That helps your provider decide if the treatment is working.
If you use NSAIDs regularly, mention it to your doctor—both can irritate the gut or affect kidneys. Always report new symptoms like dark urine, rash, unexplained fever, or chest pain. Those need prompt evaluation. For travel, pack enough medicine and keep it in original packaging with your prescription details.
Want to learn more? The September post linked patient-friendly resources and suggested questions to ask your gastroenterologist, like how long to try mesalamine before switching, and when to test kidney function. Small changes—sticking to the dose, using the right formulation, and tracking symptoms—often make the biggest difference.
Curious about other posts from September 2024 or want the full patient story with practical checklists? Browse the archive on Blueskydrugs.com for the complete article and downloadable tips you can bring to your next appointment.